The concept of a “Medical Death Note Template” might seem unsettling, conjuring images of dystopian fiction. However, in the realm of healthcare, these documents serve a profoundly important and strictly regulated purpose: ensuring the ethical and legal management of patient care when a physician is unable to continue providing it. They are a critical safeguard against medical neglect and a vital tool for protecting vulnerable patients. This document outlines the purpose, components, legal considerations, and best practices surrounding the use of a Medical Death Note Template, emphasizing its role in compassionate and responsible end-of-life care. Understanding this process is crucial for healthcare professionals, legal experts, and anyone involved in patient advocacy.
The use of a Medical Death Note Template is rooted in a complex interplay of legal frameworks, ethical guidelines, and a deep commitment to patient autonomy. It’s not about facilitating premature death; rather, it’s about providing a clear, documented pathway for transferring patient care when a physician can no longer fulfill their obligations due to illness, disability, or other circumstances. These templates are designed to offer a structured approach to communicating a patient’s wishes and ensuring continuity of care, minimizing the risk of harm and upholding the patient’s right to make informed decisions about their life. The legal landscape surrounding these documents varies by jurisdiction, making careful adherence to local regulations paramount.
The core function of a Medical Death Note Template is to facilitate a seamless and legally sound transfer of patient responsibility. When a physician determines they can no longer provide ongoing medical care – perhaps due to a debilitating illness, a relocation, or a personal emergency – they can utilize this template to formally notify the receiving physician and detail the patient’s medical history, current condition, treatment plan, and any specific instructions or preferences. This proactive approach prevents gaps in care, reduces the potential for errors, and ensures the patient’s needs are met with the utmost diligence. It’s a mechanism for prioritizing patient well-being above all else.
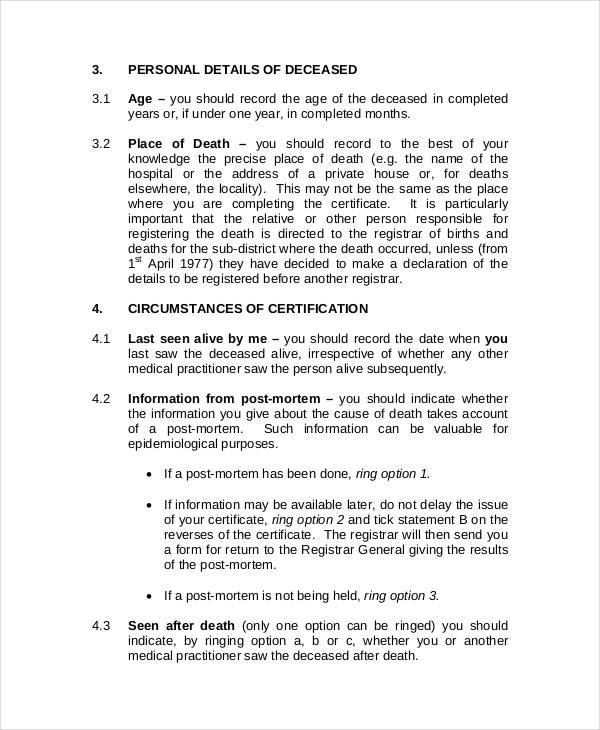
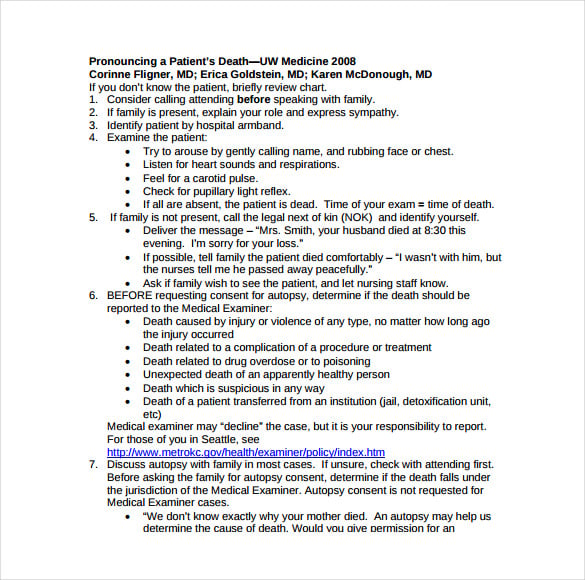
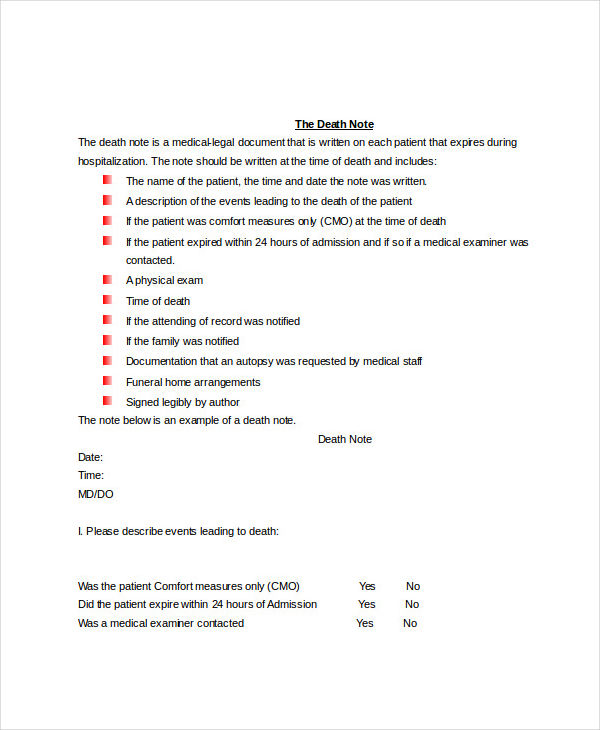
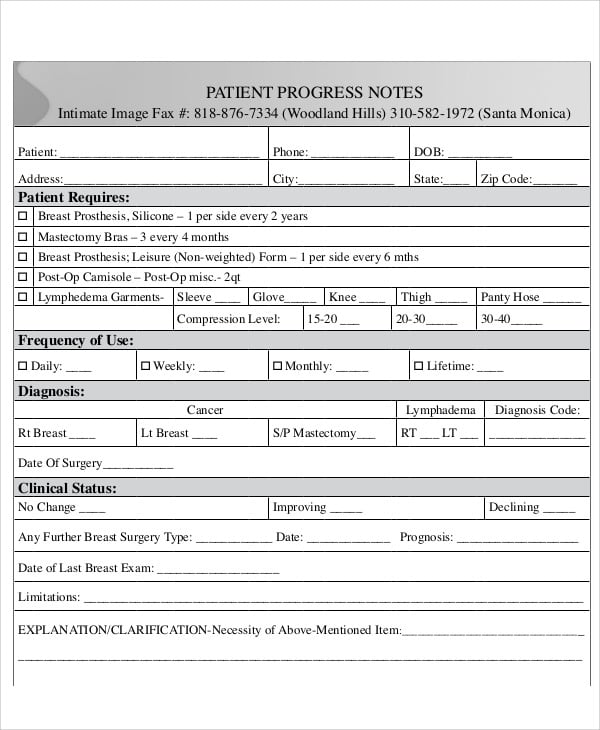
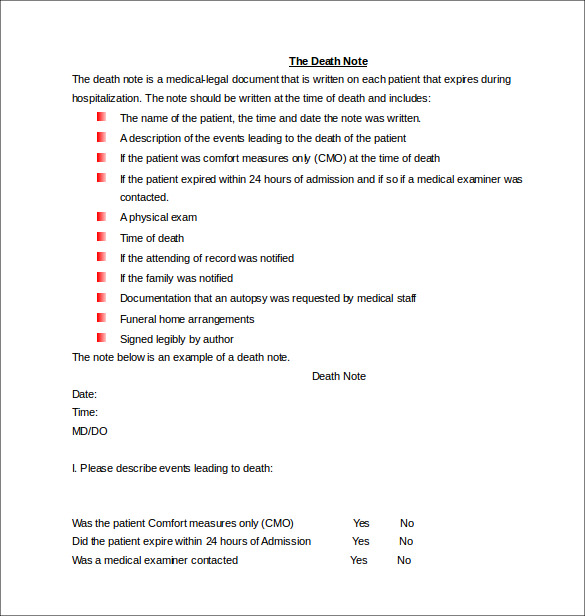
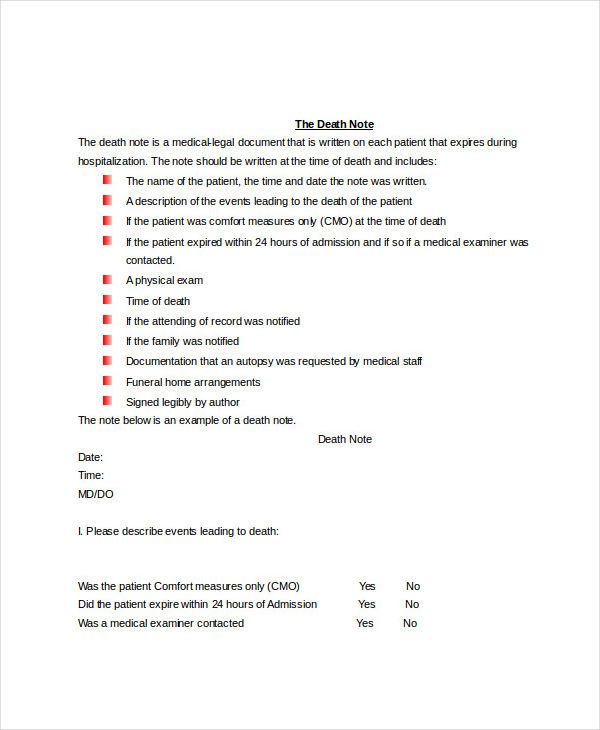
A Medical Death Note Template is a standardized document used by physicians to formally communicate the transfer of patient responsibility to another healthcare provider. It’s not a literal “death note,” but rather a detailed record of a patient’s medical status and care plan. The template typically includes sections for:
The use of a Medical Death Note Template is subject to strict legal and ethical regulations. It’s crucial for physicians to understand and comply with all applicable laws and guidelines.
Implementing a Medical Death Note Template effectively requires careful planning and adherence to best practices.
While standardized templates provide a valuable framework, it’s important to recognize that each patient’s situation is unique. A rigid adherence to a single template can sometimes be detrimental. Therefore, healthcare providers should strive for a balance between standardization and flexibility.
The role of Medical Death Note Templates is likely to evolve as healthcare continues to advance. Technological advancements, such as electronic health records and telehealth, may lead to new and improved methods for transferring patient responsibility. However, the fundamental principles of ensuring continuity of care, protecting patient autonomy, and upholding legal and ethical standards will remain paramount. Ongoing education and training for healthcare professionals are crucial to ensure the effective and responsible use of these vital documents. Furthermore, continued dialogue between legal experts, ethicists, and healthcare providers will be necessary to refine regulations and best practices.
The Medical Death Note Template is a critical tool for ensuring the ethical and legal management of patient care when a physician is unable to continue providing it. It’s a mechanism for prioritizing patient well-being, facilitating a seamless transfer of responsibility, and upholding the patient’s right to make informed decisions about their life. By understanding the purpose, components, legal considerations, and best practices surrounding these templates, healthcare professionals can play a vital role in providing compassionate and responsible end-of-life care. Continued vigilance, adherence to regulations, and a commitment to patient-centered care are essential to maximizing the benefits of this important safeguard.