In the fast-paced world of healthcare, efficient documentation is paramount. Clinicians face immense pressure to provide timely and accurate patient care while simultaneously adhering to strict regulatory guidelines. A crucial tool in this process is the Brief Op Note Template, a streamlined method for capturing essential patient information quickly and effectively. This document serves as a concise record of a patient encounter, facilitating seamless communication between healthcare providers and ensuring continuity of care. Let’s delve into the intricacies of these templates, exploring their purpose, components, and best practices for utilization.
The creation and consistent use of well-designed Brief Op Note Templates have become increasingly vital for optimizing clinical workflows. They’re not simply shortcuts; they represent a strategic approach to documentation that prioritizes clarity, conciseness, and relevance. By standardizing the format, clinicians can reduce the time spent on note-taking, freeing them to focus on direct patient interaction and complex decision-making. Furthermore, these templates contribute significantly to improved patient safety, reduced medical errors, and enhanced compliance with legal and regulatory requirements. The benefits extend beyond the individual clinician, positively impacting the entire healthcare system.
The evolution of healthcare documentation reflects a broader shift towards value-based care. Instead of exhaustive narratives, the emphasis is now on capturing the essential information needed to guide treatment decisions. Brief Op Notes align perfectly with this philosophy, providing a focused summary of the patient’s condition, treatment plan, and follow-up instructions. They’re particularly useful in settings where rapid assessments and frequent encounters are common, such as urgent care, primary care clinics, and ambulatory surgery centers. Moreover, the adoption of electronic health records (EHRs) has facilitated the widespread use and customization of these templates, making them even more accessible and efficient.
This article will provide a comprehensive guide to understanding and utilizing Brief Op Note Templates. We’ll explore the various sections commonly included, discuss best practices for tailoring templates to specific clinical settings, and examine the legal and ethical considerations surrounding their use. Whether you’re a seasoned clinician or just beginning your career, this resource will equip you with the knowledge and skills to leverage these templates effectively and contribute to improved patient care. We’ll cover everything from the foundational elements to advanced strategies for optimizing your documentation process.
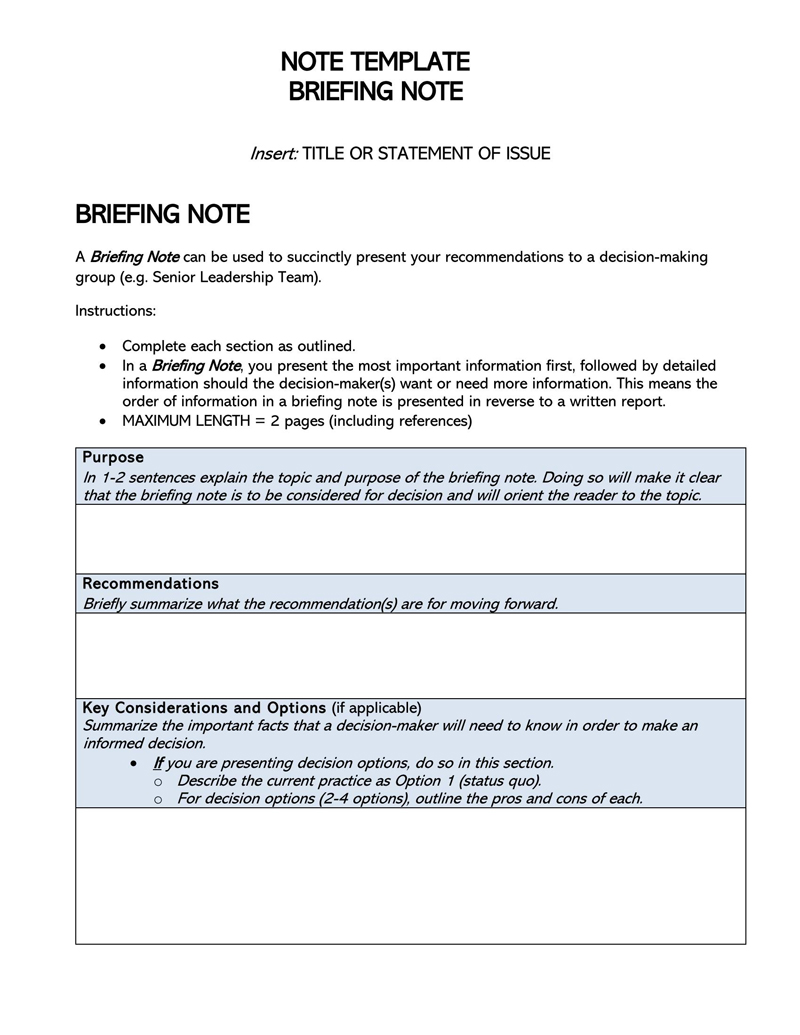
A Brief Op Note Template’s primary function is to provide a succinct, standardized record of a patient encounter. Unlike traditional progress notes, which can be lengthy and detailed, brief notes focus on the most critical information. This streamlined approach offers several key benefits:

It’s important to differentiate a Brief Op Note from a traditional progress note. While progress notes can be extensive, detailing every observation and intervention, brief notes prioritize the most relevant information. A progress note might include a detailed history, a thorough physical exam, and a lengthy discussion of treatment options. A brief note, on the other hand, typically focuses on the patient’s current condition, any changes since the last visit, the plan for the next encounter, and any pertinent lab or imaging results. The goal is to capture the “what, why, and what’s next” in a concise format.
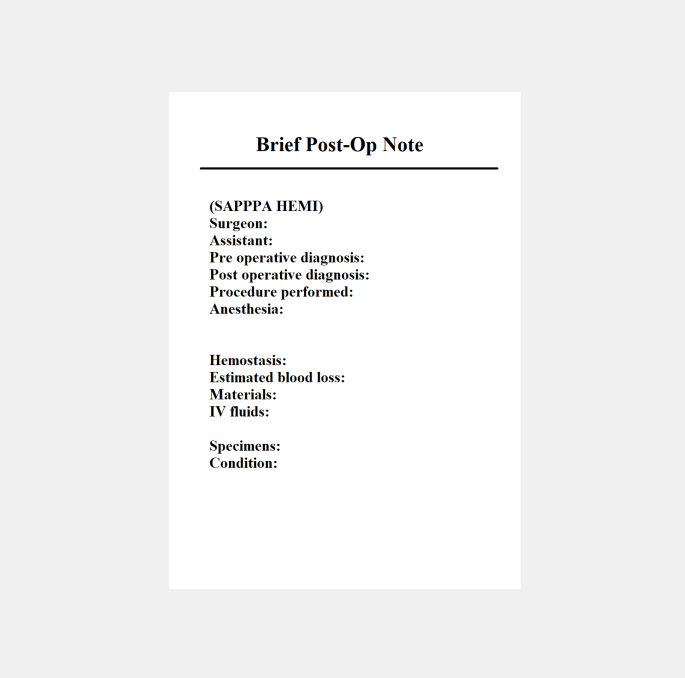
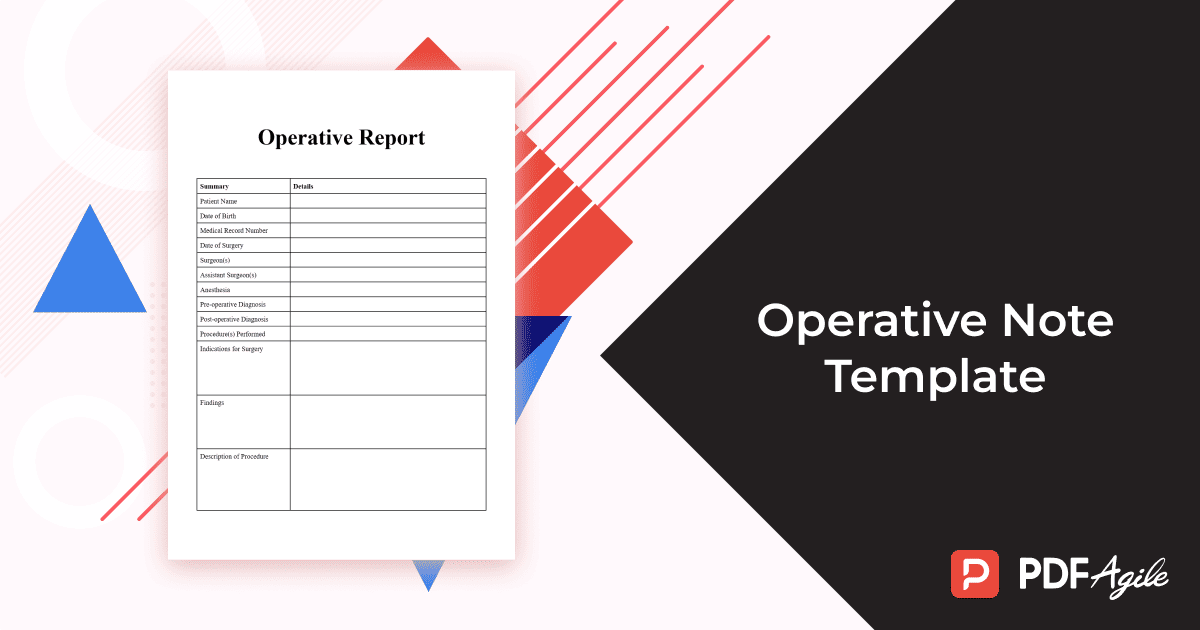
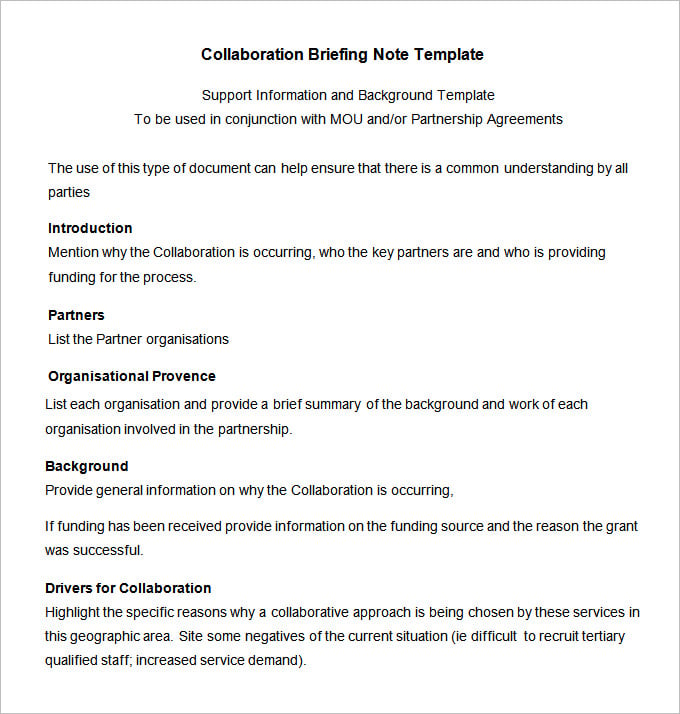
Most Brief Op Note Templates include the following core sections:
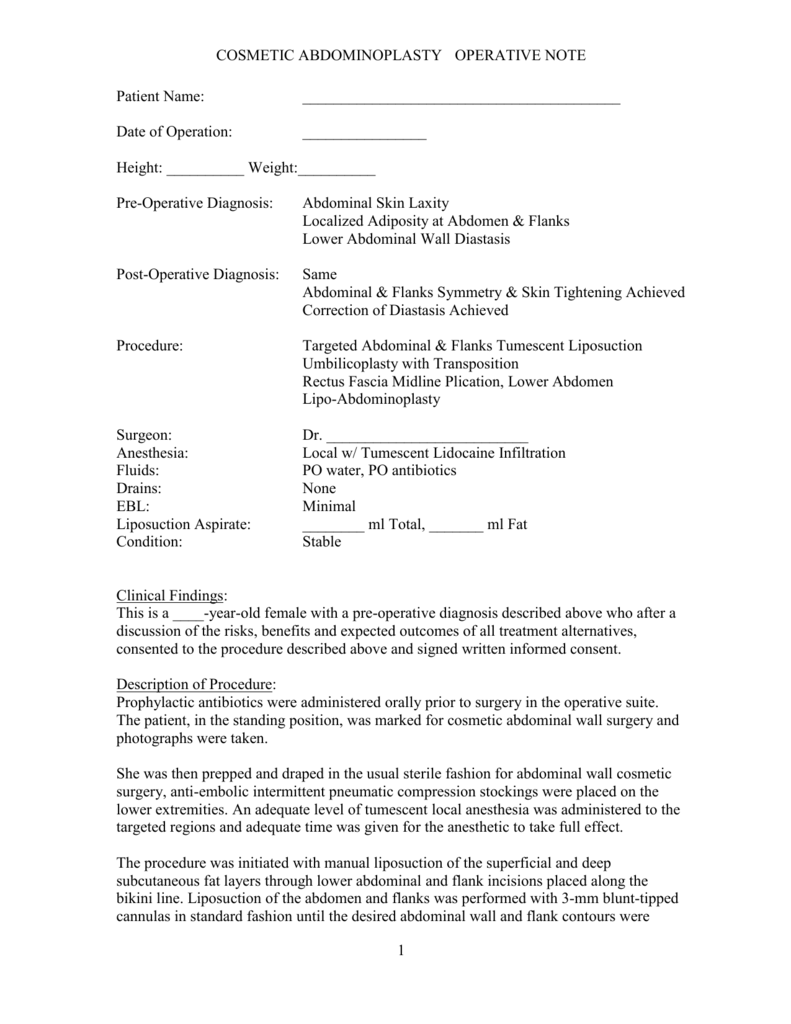
Depending on the clinical setting and the patient’s needs, additional sections may be included:

The specific content and format of a Brief Op Note Template should be tailored to the unique needs of each clinical specialty. For example:
Most modern Electronic Health Record (EHR) systems offer customizable templates for Brief Op Notes. Clinicians should take advantage of these features to create templates that align with their workflow and practice guidelines. Regularly reviewing and updating templates is crucial to ensure they remain relevant and effective. Many EHRs also allow for pre-population of data, further streamlining the documentation process.
Brief Op Note Templates should be aligned with established clinical guidelines and best practices. This ensures that all relevant information is captured and that treatment decisions are based on the latest evidence. Regularly updating templates to reflect changes in guidelines is essential for maintaining quality of care.
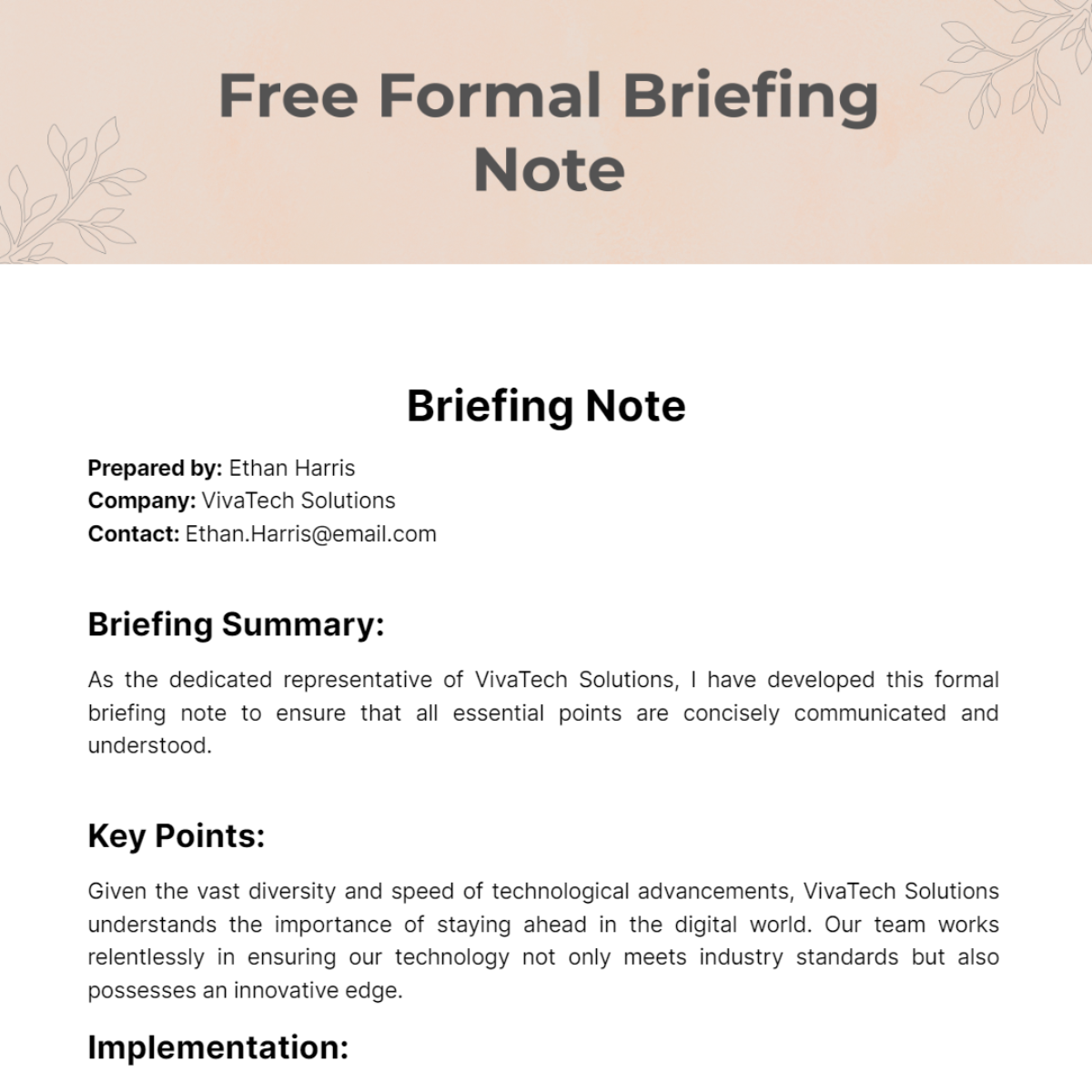
Maintaining Brief Op Note Template accuracy and completeness is paramount. All information documented must be factual and supported by objective evidence. Clinicians should avoid making subjective judgments or assumptions. Clear and concise language is crucial to minimize ambiguity and potential misunderstandings.
All documentation must comply with HIPAA regulations regarding patient confidentiality. Protected health information (PHI) should be handled with care and stored securely. Proper authorization must be obtained before disclosing patient information to third parties.
Clinicians are responsible for maintaining professional standards of documentation. Documentation should be timely, accurate, and objective. Avoid using jargon or abbreviations that may not be understood by other healthcare professionals. Always document the rationale behind treatment decisions.
Artificial intelligence (AI) and machine learning (ML) are poised to play an increasingly significant role in Brief Op Note Templates. AI-powered tools can assist with data extraction, summarization, and even automated note generation. ML algorithms can analyze patient data to identify patterns and predict potential health risks.
There’s a growing trend towards patient-centered documentation, which emphasizes the patient’s perspective and experience. Brief Op Note Templates are evolving to incorporate patient-reported outcomes and incorporate patient narratives alongside clinical findings.
Future Brief Op Note Templates will likely place a greater emphasis on measuring patient outcomes. Clinicians will be encouraged to document specific goals and track progress towards those goals. This will support value-based care models and promote accountability.
The Brief Op Note Template represents a vital advancement in healthcare documentation, offering a streamlined and efficient method for capturing essential patient information. By understanding the purpose, components, and best practices associated with these templates, clinicians can optimize their workflows, improve communication, and ultimately enhance patient care. As technology continues to evolve, Brief Op Note Templates will undoubtedly become even more sophisticated, integrating AI, machine learning, and patient-centered approaches to further revolutionize the documentation process. Consistent use of well-designed templates, coupled with a commitment to accuracy and ethical standards, is key to realizing the full potential of this valuable tool.