Navigating the world of healthcare often involves a myriad of specialized documents, each serving a critical function in patient care and medical record-keeping. Among the most recognizable and essential tools for any licensed medical professional is the prescription pad. While the digital age has introduced electronic prescribing, the tangible Blank Prescription Pad Template remains an indispensable asset for many practitioners, offering a convenient and accessible way to authorize medication, treatments, or medical devices. Understanding its components, legal implications, and best practices for its use is paramount for ensuring patient safety and maintaining regulatory compliance.
The utility of a well-designed prescription pad extends beyond merely dispensing medication. It acts as a formal communication bridge between the prescribing clinician and the pharmacist, detailing precise instructions, dosages, and patient-specific information. For patients, it provides a clear, official record of their prescribed treatment, empowering them with the information needed for their health journey.

This comprehensive guide will delve into the intricacies of a prescription pad template, exploring its fundamental elements, the legal and ethical framework governing its use, and how modern templates can be customized and integrated into various medical practices. We will uncover why a thoughtfully constructed template is not just a convenience, but a cornerstone of efficient and compliant medical practice, whether utilized in a traditional paper format or as a foundational design for digital systems.
At its core, a prescription pad serves as a legal document issued by a qualified healthcare provider, granting authorization for a patient to receive specific medications, medical devices, or therapies. Its primary purpose is to ensure the accurate and safe dispensing of treatments by clearly communicating the prescriber’s instructions to a pharmacist or other dispensing entity. Without this standardized format, miscommunication could lead to medication errors, posing significant risks to patient health and safety.
Beyond its legal standing, the prescription pad plays a crucial role in maintaining a documented chain of care. Each prescription issued becomes part of a patient’s medical record, providing a historical account of treatments, dosages, and prescribing patterns. This documentation is vital for continuity of care, allowing different healthcare providers to understand a patient’s medical history and current therapeutic regimen. It also serves as a critical reference for audits, insurance claims, and legal proceedings, underlining the importance of accuracy and completeness.

The traditional paper prescription pad also offers a sense of authority and professionalism. For many patients, receiving a physical prescription from their doctor reinforces the legitimacy and seriousness of their treatment plan. While digital alternatives are gaining traction, the familiar feel of a well-structured prescription pad continues to be a standard in many clinical settings, particularly in areas where immediate digital access might be limited or for certain types of prescriptions that require specific physical signatures or seals.
The utility of a blank prescription pad template extends across a wide spectrum of healthcare professionals and even those in related fields. Understanding who benefits highlights its pervasive importance in the medical ecosystem.
The most obvious beneficiaries are licensed doctors, physicians, and specialists in various medical fields. Whether they are general practitioners, cardiologists, dermatologists, or pediatricians, a ready-to-use template streamlines the prescribing process, ensuring all necessary legal and medical information is consistently included. This reduces the administrative burden and allows them to focus more on patient interaction and diagnosis.
Professionals outside the traditional medical doctor designation, such as dentists and optometrists, also frequently require prescription pads. Dentists prescribe antibiotics, pain relievers, and fluoride treatments, while optometrists prescribe corrective lenses and eye drops. A tailored template ensures their specific professional information and relevant prescription details are always present.
As their scope of practice expands, Nurse Practitioners (NPs) and Physician Assistants (PAs) are increasingly authorized to prescribe medication. For these vital members of the healthcare team, a standardized prescription pad template is essential for exercising their prescribing privileges legally and efficiently, often requiring specific identifiers unique to their roles.
It’s not just human medicine that relies on prescriptions. Veterinarians routinely prescribe medications for animals. A blank prescription pad template designed for veterinary use ensures appropriate information for animal patients, including species, weight, and specific dosing instructions, is captured accurately.
While not yet authorized to prescribe independently, medical students and residents often use mock prescription pads or templates for educational purposes. This allows them to practice the critical skill of writing clear, compliant prescriptions under supervision, preparing them for their future roles as independent prescribers.
From small private practices to large hospital systems, healthcare facilities and clinics benefit from having standardized templates. This ensures uniformity across all prescribers within the organization, aids in inventory management of physical pads, and helps maintain a consistent brand image and adherence to internal policies.
The use of a prescription pad is not merely a procedural task; it is steeped in significant legal and ethical responsibilities. Any misstep can lead to serious consequences, including legal penalties, professional disciplinary actions, and, most importantly, patient harm. Therefore, understanding and adhering to the regulatory framework is paramount.
Prescribing practices are governed by a complex web of state and federal laws. Federal laws, such as those enforced by the Drug Enforcement Administration (DEA), dictate the prescribing of controlled substances, requiring specific DEA registration numbers on all such prescriptions. State laws, often managed by medical boards or pharmacy boards, outline specific requirements for prescription content, format, and security features (e.g., tamper-resistant pads). A blank prescription pad template must be designed to accommodate all these mandatory fields and features relevant to the prescriber’s jurisdiction.
The prescriber holds ultimate responsibility for every prescription issued. This includes ensuring the prescription is medically appropriate, the dosage is correct, potential drug interactions have been considered, and the patient understands the instructions. Ethical obligations dictate that prescriptions should only be issued for legitimate medical purposes, avoiding any conflict of interest or abuse of authority. The template serves as a tangible record of this responsibility.
A critical legal and ethical concern is the prevention of prescription fraud and tampering. Historically, prescription pads have been targets for individuals seeking to illegally obtain controlled substances. This has led to the development of tamper-resistant prescription pads, which often feature:
* Chemically altered paper that changes color if erased.
* Void pantographs that reveal the word “VOID” when photocopied.
* Reflective security watermarks.
* Serial numbering for tracking.
* Microprinting that is legible only under magnification.
* Erasure protection.
A robust blank prescription pad template must incorporate or account for these security features, especially when physical pads are printed. For electronic templates, robust digital security measures and authentication protocols are equally crucial.
Prescriptions contain Protected Health Information (PHI), making HIPAA compliance a non-negotiable requirement. While the prescription pad itself isn’t the sole repository of PHI, its handling, storage, and disposal must adhere to privacy regulations. This includes ensuring pads are not left unattended where they could be stolen, and securely disposing of outdated or unused pads. Electronic prescribing systems built upon a template must be equally secure to prevent unauthorized access to patient data.
Beyond the law, ethical prescribing mandates a commitment to patient well-being. This involves prudent prescribing, avoiding unnecessary medications, considering the financial burden on patients, and educating patients thoroughly about their prescriptions. The act of filling out a prescription, guided by a comprehensive template, reinforces these ethical duties by promoting clarity, accuracy, and thoroughness.
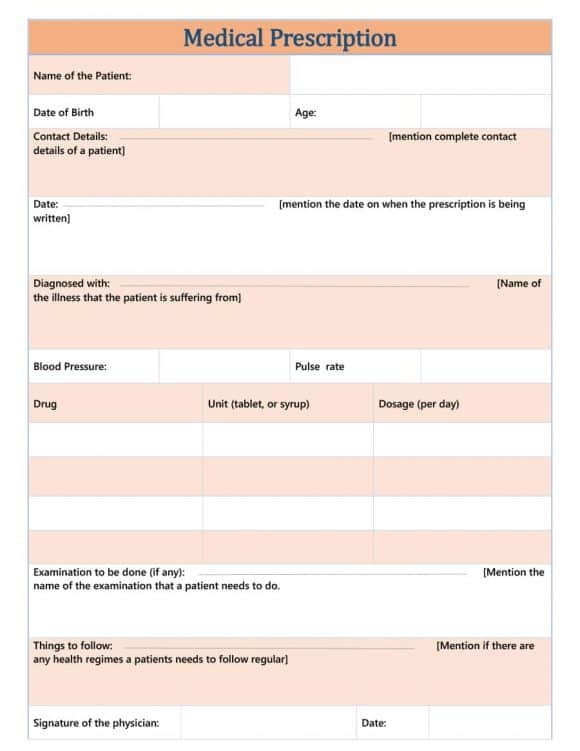
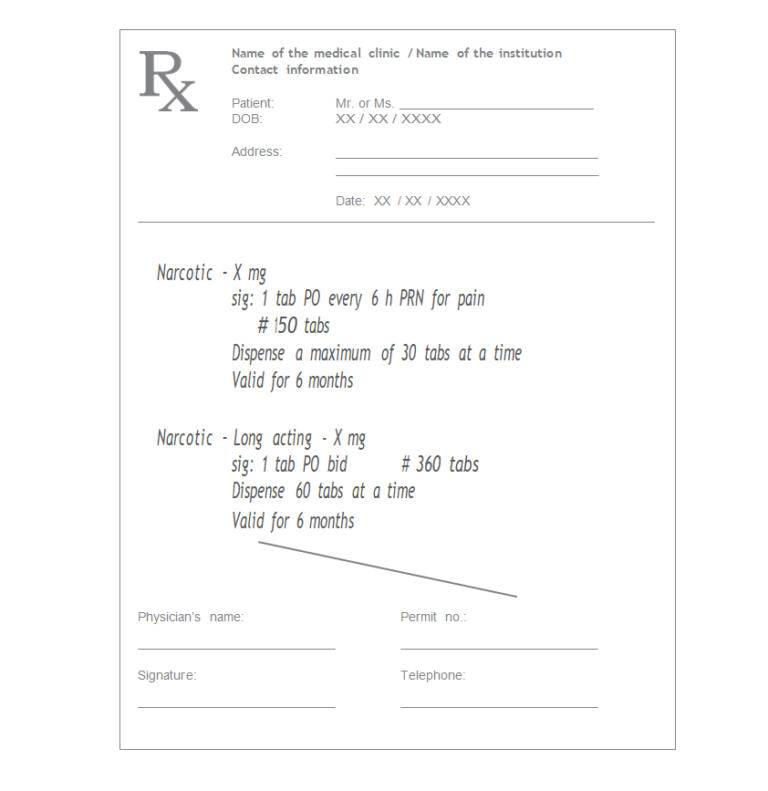
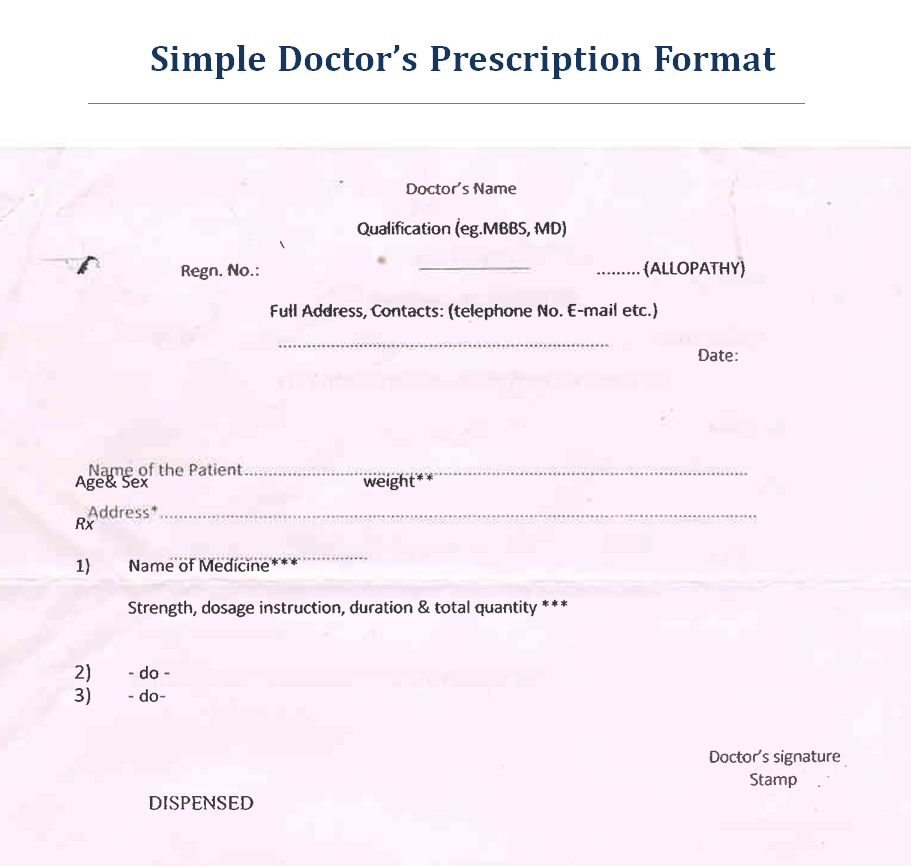
A truly effective blank prescription pad template is more than just a piece of paper with lines; it’s a meticulously designed tool that facilitates clarity, compliance, and patient safety. Each element serves a specific purpose, contributing to the overall functionality and legality of the prescription.
This section identifies the medical professional authorizing the prescription. It typically includes:
* Full Name and Credentials: Dr. Jane Doe, MD, or Jane Doe, APRN.
* Practice Name and Address: The official name and physical location of the clinic or hospital.
* Contact Information: Phone number for the pharmacy to verify the prescription if needed.
* License Number: The state-issued medical license number.
* DEA Registration Number: Crucial for prescribing controlled substances, issued by the Drug Enforcement Administration.
* NPI Number: National Provider Identifier, a standard unique identification number for healthcare providers.
Accurate patient identification is vital to prevent medication errors. This section should include:
* Full Name: First and last name.
* Date of Birth: To confirm identity and help with age-appropriate dosing.
* Address: Often included for identification, especially for controlled substances.
This is the core of the prescription, detailing the medication or treatment.
* Drug Name: Generic preferred, but brand name if medically necessary, with clear specification.
* Dosage Strength: E.g., 250 mg, 10 mcg/mL.
* Formulation: E.g., tablet, capsule, liquid, cream, injection.
* Quantity: Total amount to be dispensed (e.g., #30 tablets, 1 bottle).
* Directions for Use (Sig): Clear, concise instructions for the patient on how to take the medication, including route, frequency, and any special instructions (e.g., “Take one tablet by mouth twice daily,” “Apply thin layer to affected area once daily”).
* Refills: Number of authorized refills (e.g., “0 refills,” “3 refills,” “PRN for 1 year”).
* Dispense as Written (DAW) / Brand Medically Necessary: A check box or line indicating if a specific brand-name medication is required, overriding generic substitution.
These elements formalize the prescription and establish its validity.
* Date Issued: The specific date the prescription was written. This is critical for expiration and refill calculations.
* Prescriber’s Signature: The handwritten signature of the prescribing clinician, confirming authenticity. For electronic prescriptions, this is replaced by a secure digital signature.
As discussed, these are crucial for preventing fraud and tampering:
* Tamper-Resistant Features: Often visible warnings, special paper, microprinting.
* Unique Serial Number: For tracking and inventory control.
* Barcode (Optional): Can be used for internal tracking or integration with pharmacy systems.
Depending on the specialty or practice, additional fields might be useful:
* Diagnosis Code (ICD-10): Sometimes required by insurance or for specific medications.
* Allergies: A small section to note known patient allergies.
* Weight/Age: Especially for pediatric or geriatric patients, to aid in dosage verification.
* “May Substitute” / “No Substitution” Checkbox: Another way to indicate generic preference.
A well-designed blank prescription pad template thoughtfully integrates all these components into a clear, legible, and logical layout, minimizing errors and maximizing efficiency for both the prescriber and the pharmacist.
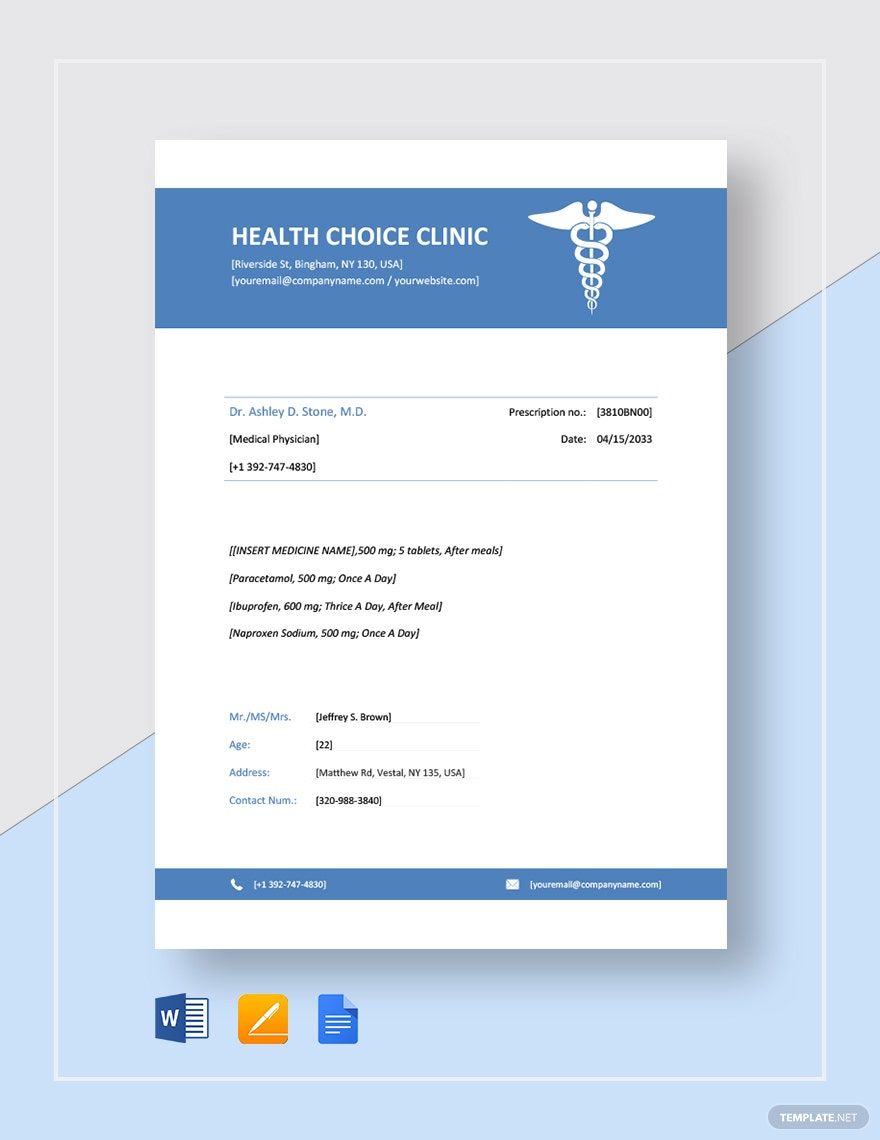
Creating a blank prescription pad template that is both functional and compliant requires careful consideration of design, content, and the specific needs of your practice. Customization allows you to tailor the template to your specialty, brand, and workflow, ensuring maximum efficiency and professionalism.
The format of your template will depend on whether you plan to use physical pads or integrate it into an electronic prescribing system.
* Physical Pads: Typically involve a standard size (e.g., 4″ x 5.5″ or 5.5″ x 8.5″). The layout should be intuitive, with clear demarcations for each section. Adequate white space is crucial for readability and ease of writing.
* Digital Templates: Offer more flexibility in layout but must prioritize ease of data entry and integration with Electronic Health Records (EHR) systems. Drop-down menus, auto-fill functions, and structured fields enhance efficiency.
Regardless of the format, prioritize a logical flow from top to bottom, typically starting with prescriber and patient information, followed by the medication details, and ending with date and signature.
Your prescription pad is a direct representation of your practice. Incorporating your practice’s logo and contact information prominently at the top lends a professional and authoritative appearance. Consistency in font choices and overall aesthetic with your other practice materials reinforces your brand identity. While customization is key, ensure that branding elements do not obscure critical information or violate any regulatory requirements regarding font size or clarity.
Every practice has unique needs. Your template should reflect these:
* Specialty-Specific Fields: For an ophthalmologist, a section for “OD/OS” (right eye/left eye) might be beneficial. A pediatrician might benefit from a field for patient weight.
* Commonly Prescribed Medications: While you won’t pre-fill medications, you might design the Rx section to accommodate common prescribing patterns in your specialty, perhaps with more space for specific instructions for complex regimens.
* Clinic-Specific Instructions: Some templates include a small footer for pharmacy instructions, such as preferred local pharmacies or specific billing codes if applicable.
If you’re designing a physical blank prescription pad template, liaising with a specialized printer is crucial. They can advise on and implement various security features:
* Tamper-Resistant Paper: This is a fundamental requirement in many states, often with specific federal guidelines for controlled substances.
* Sequential Numbering: This helps in tracking and auditing, deterring theft or misuse of pads.
* Microprinting and Watermarks: These subtle features add layers of security that are difficult for counterfeiters to replicate.
For those moving towards or utilizing electronic prescribing, the blank prescription pad template translates into the underlying structure of their e-prescribing software.
* Integration with EHR: The template should seamlessly pull patient demographics from the EHR and push prescription details back into the patient’s chart.
* Drug Databases: Integration with comprehensive drug databases (e.g., Surescripts) allows for easy drug selection, dosage lookup, and automated interaction checks.
* Electronic Signatures: Secure, legally compliant electronic signature functionalities are paramount.
* Audit Trails: Digital templates must include robust audit trails to track who accessed and prescribed what, when, and for whom.
Designing and customizing your template, whether for physical or digital use, is an ongoing process. Regular review of state regulations and best practices ensures your template remains compliant, efficient, and a valuable asset in patient care.
The landscape of medical prescribing has evolved significantly, presenting healthcare professionals with two primary approaches: the traditional printable prescription pad and the increasingly prevalent digital e-prescribing system. Each has its distinct advantages and considerations, particularly when considering a blank prescription pad template.
Advantages:
* Simplicity and Accessibility: Printable pads require minimal technology and are easy to use, especially in areas with unreliable internet access or during power outages.
* Familiarity: Many patients and pharmacists are accustomed to the physical format, which can feel more tangible and authoritative.
* Flexibility for Certain Situations: Ideal for house calls, remote clinics, or when a quick, on-the-spot prescription is needed without access to a computer.
* Specific Legal Requirements: Some controlled substances or certain medical devices may still require a physical, tamper-resistant prescription in specific jurisdictions.
Disadvantages:
* Security Risks: Susceptible to loss, theft, and forgery if not properly secured and managed. Tamper-resistant features mitigate this but don’t eliminate it entirely.
* Manual Processes: Requires manual writing, which can be time-consuming and prone to errors (illegible handwriting).
* Lack of Integration: Does not directly integrate with EHR systems, requiring manual entry of prescription data into patient records, leading to potential data entry errors and redundancy.
* Environmental Impact: Paper consumption and associated printing processes.
A blank prescription pad template for printing needs to be designed with physical constraints and security features (as discussed previously) in mind, ensuring it can be reproduced by a specialized printer onto compliant paper.
Advantages:
* Enhanced Safety: Reduces medication errors due to illegible handwriting, provides real-time drug interaction alerts, allergy checks, and appropriate dosing guidance.
* Efficiency: Streamlines the prescribing workflow with auto-filled patient data, quick drug selection, and direct transmission to pharmacies.
* Security and Auditability: Robust encryption, access controls, and comprehensive audit trails protect patient data and deter fraud. DEA-compliant electronic prescribing for controlled substances (EPCS) ensures high-level security.
* Integration with EHR: Seamlessly updates patient records, improving data accuracy and continuity of care.
* Convenience for Patients: Eliminates the need for patients to drop off paper prescriptions, potentially reducing wait times at pharmacies.
* Environmental Friendliness: Reduces paper waste.
Disadvantages:
* Initial Setup Cost: Implementing an e-prescribing system and integrating it with existing EHR can be expensive.
* Learning Curve: Requires training for staff and prescribers.
* Technical Dependencies: Relies on stable internet connection, power, and functional hardware.
* System Downtime: Any technical issues or system failures can disrupt prescribing.
For digital systems, the blank prescription pad template forms the structural backbone of the software interface. It dictates the fields available, their order, and how data is captured and transmitted. The design principles still apply, but they are translated into user interface (UI) and user experience (UX) elements within the software, focusing on intuitive navigation, data validation, and seamless backend integration.
Many practices adopt a hybrid approach, using e-prescribing for the majority of their prescriptions while retaining a small supply of secure, tamper-resistant printable pads for specific situations. This strategy offers the best of both worlds, leveraging the efficiency and safety of digital systems while maintaining a fallback for unforeseen circumstances or specific regulatory requirements. Regardless of the primary method, a well-defined blank prescription pad template (whether physical or digital) remains crucial for consistent, compliant, and patient-centric prescribing.
The integrity of a prescription pad, whether physical or digital, is paramount for patient safety and legal adherence. Ensuring robust security measures and strict compliance with regulations is a continuous responsibility for every prescriber and healthcare facility.
For traditional paper prescription pads, security starts with the physical attributes of the pad itself:
* Tamper-Resistant Features: As previously discussed, these include void pantographs, chemical alteration, microprinting, and security watermarks. Many states mandate the use of such pads for all prescriptions, particularly for controlled substances.
* Sequential Numbering: Each pad and prescription within it should have a unique, sequential number. This aids in tracking, auditing, and quickly identifying missing or stolen pads.
* Secure Storage: Unused prescription pads must be stored in a locked, secure location, inaccessible to unauthorized personnel. They should never be left unattended on desks or in examination rooms.
* Accountability and Inventory: A robust system for tracking the issuance and use of prescription pads is crucial. This includes logging when pads are received, who they are issued to, and regular audits to ensure all pads are accounted for.
Electronic Prescribing of Controlled Substances (EPCS) has even more stringent security requirements than non-controlled e-prescribing:
* Identity Proofing: Prescribers must undergo a rigorous identity proofing process to verify their identity.
* Two-Factor Authentication (2FA): Access to the e-prescribing system and the act of signing a controlled substance prescription requires two distinct authentication factors (e.g., a password and a fingerprint, or a token and a PIN).
* Audit Trails: Every action within the system, from login to prescription transmission, is logged and auditable, creating an irrefutable record.
* System Certifications: EPCS software must be certified by a third-party auditor to meet DEA requirements.
* Secure Transmission: Prescriptions are transmitted electronically through secure, encrypted networks (e.g., Surescripts) directly to the pharmacy.
Both physical and digital prescription processes must strictly adhere to HIPAA regulations:
* Data Minimization: Only necessary patient information should be included on the prescription.
* Access Control: Only authorized personnel should have access to prescription information, whether written or electronic.
* Secure Disposal: Physical prescriptions or outdated pads containing PHI must be shredded or disposed of through HIPAA-compliant methods. Digital data must be securely erased from systems when no longer needed, following data retention policies.
* Training: All staff involved in handling prescriptions must be trained on HIPAA privacy and security rules.
A proactively designed blank prescription pad template, coupled with rigorous procedural safeguards and ongoing education, forms the bedrock of a secure and compliant prescribing practice, protecting both the patient and the prescriber.
Creating and effectively utilizing a blank prescription pad template involves several steps, from design to implementation, ensuring it meets both regulatory requirements and the practical needs of a busy medical practice.
Before designing anything, thoroughly research all applicable state and federal regulations concerning prescription pads. This includes:
* Mandatory fields: What information must be present (prescriber info, patient info, drug details, signature, date).
* Security features: Are tamper-resistant pads required? What specific features must they have (e.g., void pantograph, microprinting)?
* Controlled substance requirements: Any special formatting or numbering for Schedule II-V drugs.
* Font size and legibility standards: To ensure clarity.
Consult your state’s Board of Medicine or Pharmacy website, and federal DEA guidelines.
Using design software (like Adobe InDesign, Microsoft Word, or even specialized prescription pad software), begin laying out your template.
* Header: Place your practice name, logo, full prescriber name, credentials (MD, DO, APRN, PA-C), NPI, DEA number (if applicable), address, and phone number at the top.
* Patient Section: Create clear fields for patient’s full name, date of birth, and possibly address.
* Rx Section: Designate ample space for the drug name, strength, dosage form, quantity, directions (Sig), and number of refills. Include checkboxes for “Dispense as Written” / “Brand Medically Necessary” and “May Substitute.”
* Footer: Include a clear line for the date and a dedicated space for the prescriber’s signature. You might also add small print for “State Law Requires Tamper-Resistant Pad” or other disclaimers.
* Spacing and Readability: Ensure adequate spacing between fields and use clear, professional fonts that are easily legible. Avoid clutter.
If opting for physical pads, this is where you engage with a professional printer specializing in secure medical documents.
* Choose Tamper-Resistant Paper: Select paper with the required security features (e.g., color-changing, “VOID” message when copied, chemical void).
* Sequential Numbering: Work with the printer to implement unique, sequential numbering on each prescription form.
* Additional Features: Discuss microprinting, watermarks, or other advanced security measures.
For digital templates, ensure your e-prescribing software is DEA-certified for EPCS and implements all necessary security protocols (2FA, audit trails).
Before mass production or full digital implementation:
* Legal Review: Have a legal expert or compliance officer review the template to ensure it meets all current regulations.
* Peer Review: Ask colleagues or pharmacists to review the template for clarity, ease of use, and completeness.
* Test Run: For physical pads, write a few mock prescriptions to ensure everything aligns correctly and is legible. For digital, conduct thorough user acceptance testing.
Once your blank prescription pad template is ready for use:
* Training: Train all staff and prescribers on the correct and secure use of the pads/system, including how to fill them out accurately, handle them securely, and dispose of them properly.
* Inventory Control: Regularly audit your physical pad inventory to account for all forms. For digital systems, monitor access logs.
* Regular Updates: Regulations change. Periodically review your template to ensure it remains compliant with the latest state and federal laws. Update it as needed to reflect changes in your practice or in prescribing standards.
* Electronic Integration: If using an e-prescribing system, continuously ensure its seamless integration with your EHR and pharmacy networks, and address any technical issues promptly.
By following these steps, healthcare providers can ensure their prescription pads are not only compliant and secure but also efficient tools that support optimal patient care.
The Blank Prescription Pad Template, whether in its traditional paper format or as the underlying structure of a sophisticated e-prescribing system, remains a cornerstone of modern medical practice. It bridges the critical gap between diagnosis and treatment, providing a legally recognized, clear, and standardized method for healthcare professionals to authorize medications and therapies. Its importance is multifaceted, encompassing legal compliance, patient safety, communication clarity, and the efficient flow of information within the complex healthcare ecosystem.
From understanding the specific elements that comprise an effective template—such as precise prescriber and patient data, detailed medication instructions, and essential security features—to navigating the intricate web of state and federal regulations, the responsibility of proper prescription pad management is substantial. The decision between a printable pad and a digital system often depends on the practice’s needs, technological infrastructure, and specific legal requirements, with many opting for a hybrid approach that leverages the strengths of both.
Ultimately, a thoughtfully designed, regularly updated, and securely managed blank prescription pad template is more than just an administrative tool; it is a testament to a healthcare provider’s commitment to professionalism, accuracy, and the highest standards of patient care. By prioritizing its integrity and adhering to best practices, practitioners can continue to ensure safe, effective, and compliant prescribing, safeguarding both their patients and their practice.