Maintaining accurate and thorough documentation is paramount in the field of mental health. Clinicians rely on detailed records not only for continuity of care but also for legal and ethical considerations, billing accuracy, and effective communication with other healthcare professionals. A crucial tool in this process is the Soap Notes Mental Health Template, a standardized format for recording and organizing patient information. This template provides a structured approach to documenting subjective experiences, objective observations, assessments, and plans for treatment, ensuring a comprehensive and easily understandable record of each session. Without a consistent and well-maintained system like this, crucial details can be overlooked, potentially impacting the quality of care provided.
The SOAP note method, originally developed in the medical field, has been adapted and refined for use in mental health settings. It’s a widely accepted and recognized format, making it easier for professionals to share information and collaborate effectively. Utilizing a standardized template streamlines the documentation process, saving valuable time and reducing the risk of errors. This is particularly important in today’s fast-paced healthcare environment where clinicians often manage a large caseload.

Beyond the practical benefits of organization and efficiency, a well-crafted SOAP note serves as a powerful tool for reflecting on clinical practice. By systematically documenting each session, clinicians can identify patterns, track progress, and refine their treatment approaches. This reflective process is essential for ongoing professional development and ensuring the delivery of evidence-based care.
.png)
Ultimately, the goal of using a Soap Notes Mental Health Template isn’t simply to fulfill a documentation requirement; it’s to enhance the quality of care provided to patients and to support the clinician’s ability to deliver effective and ethical treatment.
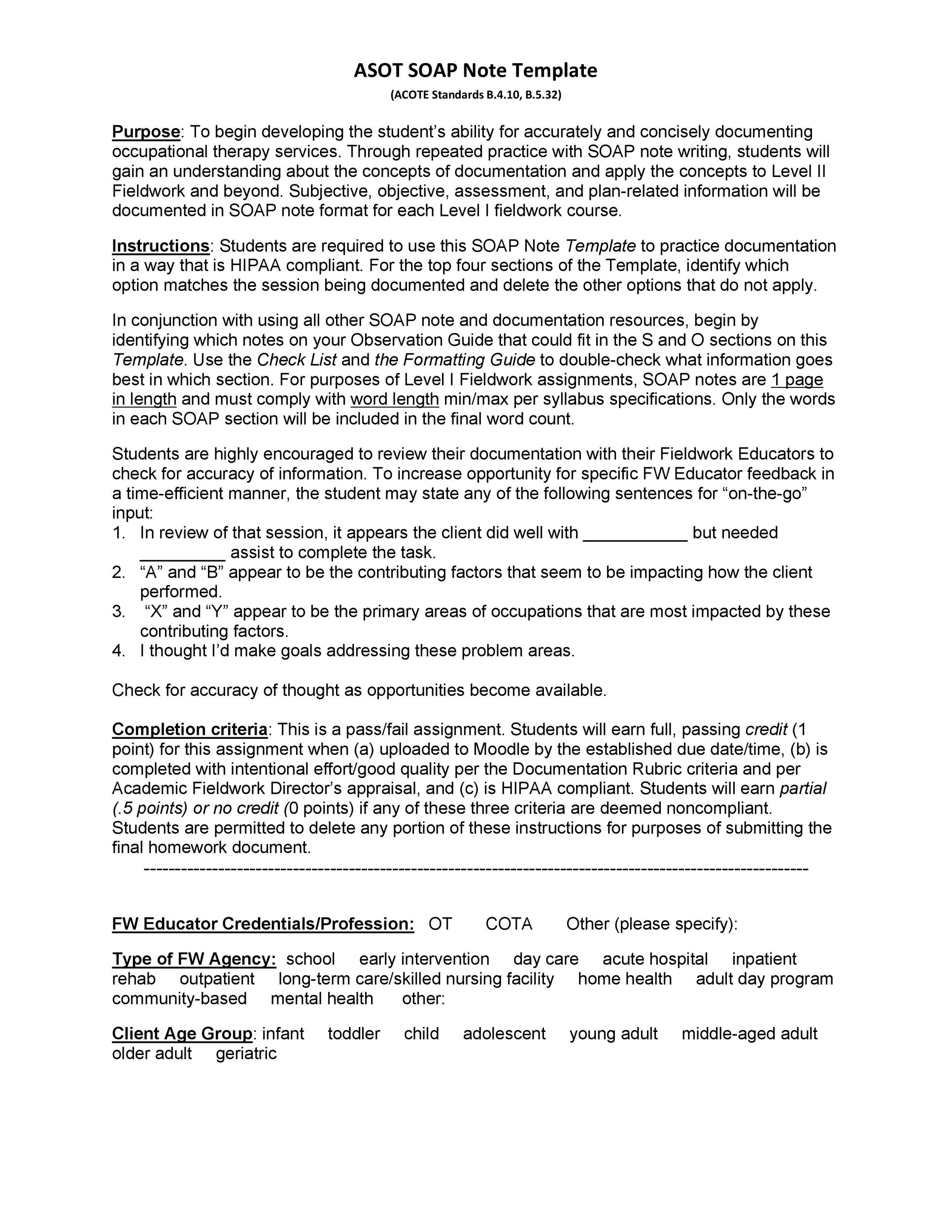
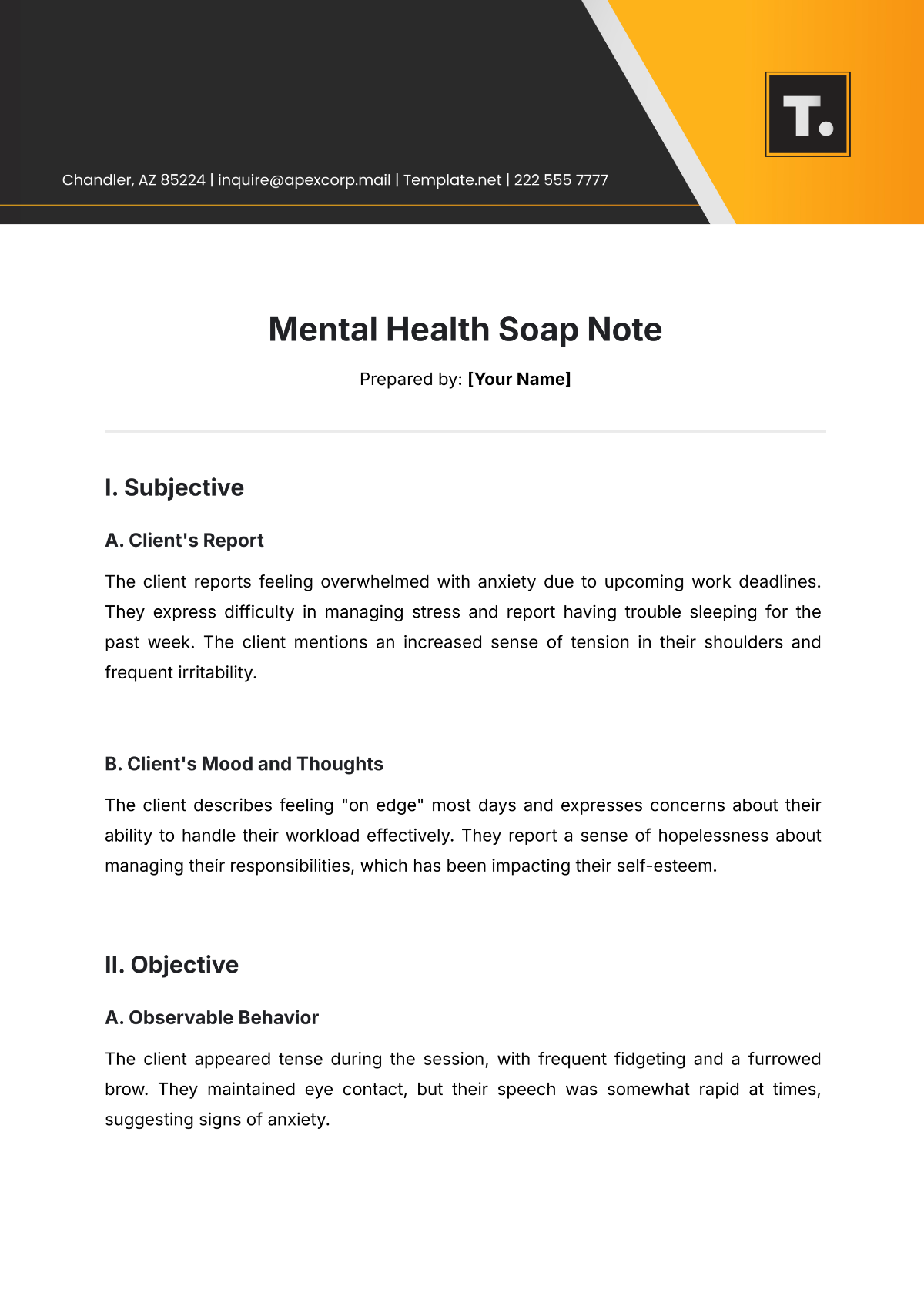
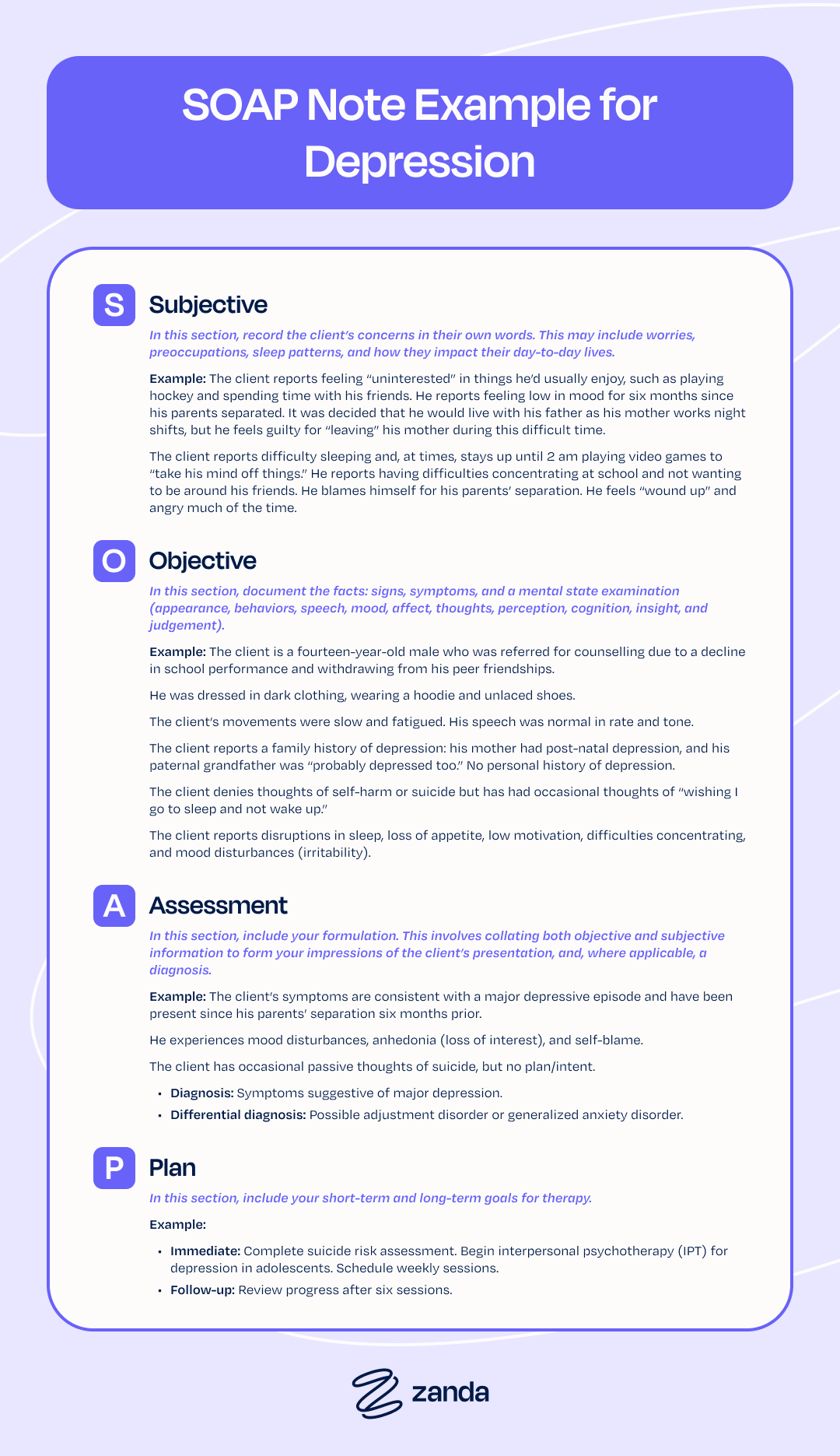
The acronym SOAP stands for Subjective, Objective, Assessment, and Plan. Each section serves a distinct purpose in documenting a patient’s mental health status and the course of treatment. Understanding the nuances of each component is crucial for creating effective and legally sound notes.
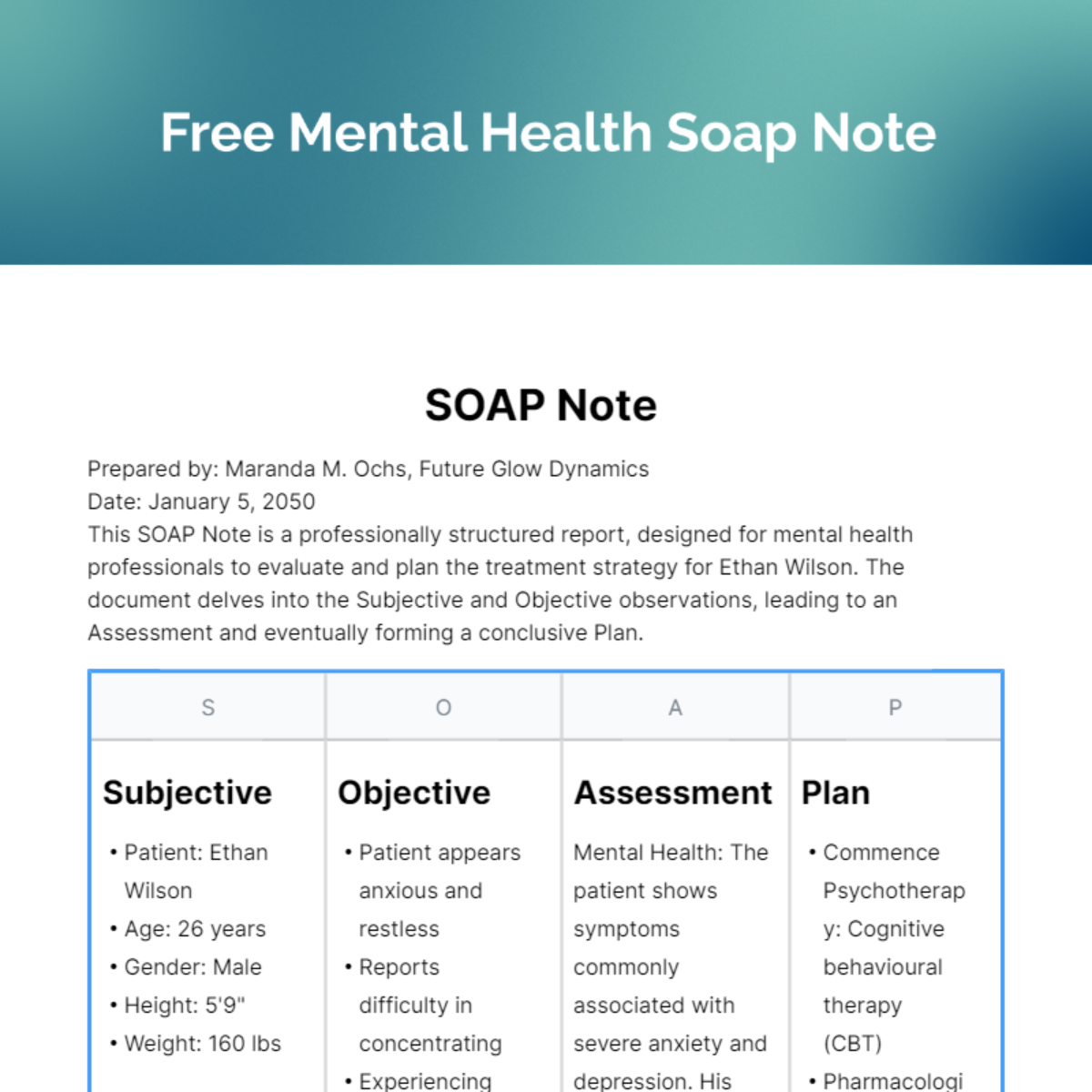
This section captures the patient’s own perspective – their feelings, thoughts, and experiences. It’s documented in the patient’s own words as much as possible, using direct quotes when appropriate. Key elements to include in the subjective section are the chief complaint (the primary reason the patient is seeking treatment), a description of their current symptoms, relevant history (including past mental health issues, medical conditions, and substance use), and any significant life events or stressors. Avoid making interpretations or diagnoses in this section; simply record what the patient reports.
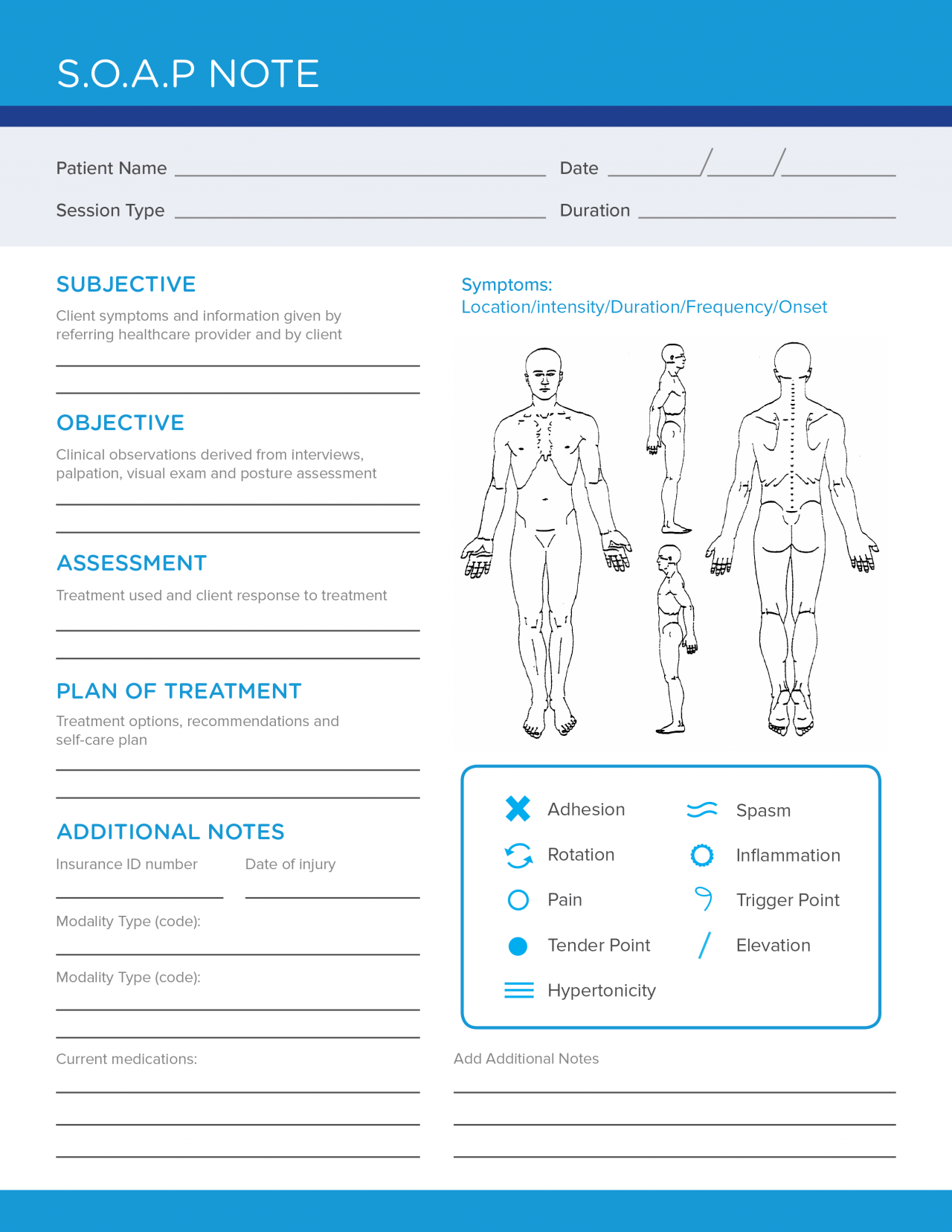
The objective section contains factual, observable data. This includes the clinician’s observations of the patient’s appearance, behavior, mood, and affect. It also includes results from any standardized assessments or tests administered during the session. Unlike the subjective section, the objective section should be free of personal opinions or interpretations. Focus on concrete, measurable data. For example, instead of writing “Patient appeared sad,” write “Patient exhibited slowed speech, reduced eye contact, and a flat affect.”
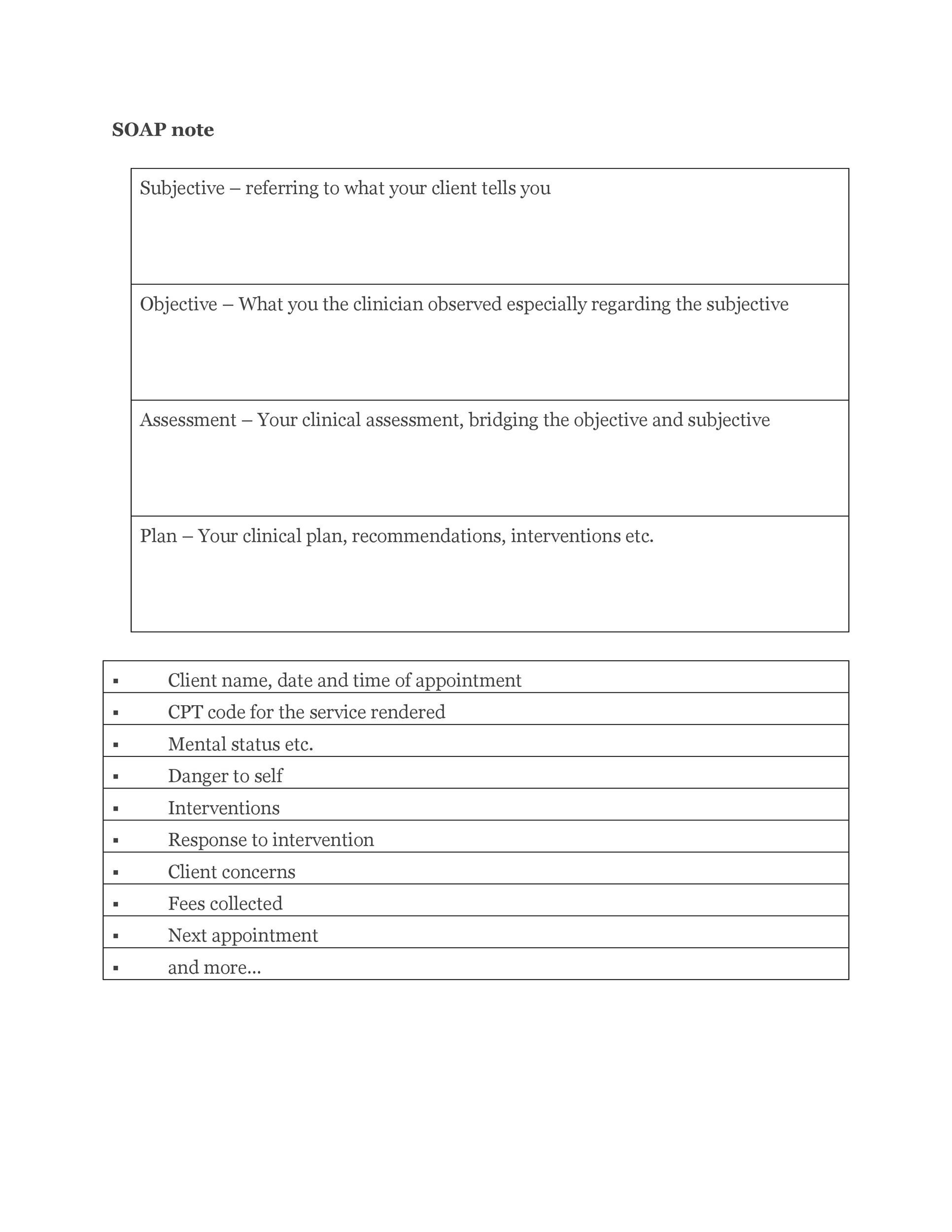
This is where the clinician synthesizes the information from the subjective and objective sections to form a clinical impression. This section includes the clinician’s diagnosis (using DSM-5 criteria), a summary of the patient’s current functioning, and an analysis of the factors contributing to their difficulties. The assessment should be concise and focused, clearly articulating the clinician’s understanding of the patient’s presenting problems.
The plan section outlines the next steps in treatment. This includes specific interventions, such as therapy techniques, medication adjustments (if applicable), and referrals to other services. The plan should be SMART – Specific, Measurable, Achievable, Relevant, and Time-bound. It should also include any homework assignments or recommendations for the patient.
There are numerous Soap Notes Mental Health Template options available, ranging from simple paper-based forms to sophisticated electronic health record (EHR) systems. The best choice depends on the clinician’s individual needs, practice setting, and budget.
These are a cost-effective option for clinicians who prefer a traditional approach to documentation. Paper templates can be easily customized to fit specific practice needs. However, they can be time-consuming to maintain and may be prone to errors or loss.
Digital templates offer greater flexibility and ease of use than paper-based forms. They can be easily stored, shared, and backed up. Many free and paid templates are available online. However, they may not integrate with other practice management systems.
EHR systems provide a comprehensive solution for managing patient records, including SOAP notes. They offer features such as automated billing, scheduling, and reporting. While EHR systems can be expensive to implement, they can significantly improve efficiency and accuracy. Look for EHRs specifically designed for behavioral health to ensure they include features tailored to mental health documentation.
Regardless of the template you choose, it’s important to customize it to meet your specific needs and the requirements of your practice.
Include your practice name, address, and contact information on the template. You may also want to add a section for patient demographics and insurance information.
Adjust the assessment and plan sections to reflect your theoretical orientation and preferred treatment approaches. For example, a cognitive-behavioral therapist might include specific sections for identifying and challenging maladaptive thoughts.
Add sections for standardized assessments that you routinely administer, such as the Beck Depression Inventory or the Generalized Anxiety Disorder 7-item scale.
Writing clear, concise, and accurate SOAP notes is essential for providing high-quality mental health care.
Avoid making subjective judgments or interpretations. Stick to observable data and the patient’s own words.
Avoid jargon and technical terms that the patient or other healthcare professionals may not understand.
Provide enough detail to accurately convey the patient’s condition and the course of treatment.
Protect patient privacy by adhering to HIPAA regulations and ethical guidelines.
Ensure that all notes are properly dated and signed.
The rise of telehealth has presented new considerations for documentation. While the core principles of SOAP note writing remain the same, clinicians need to adapt their approach to account for the unique aspects of virtual care.
Pay close attention to non-verbal cues, such as facial expressions and body language, and document them in the objective section.
Document any technical difficulties that may have impacted the session, such as poor audio or video quality.
Confirm the patient’s location at the beginning of the session to ensure compliance with state regulations.
The Soap Notes Mental Health Template is an indispensable tool for mental health professionals. By providing a structured and standardized format for documentation, it enhances the quality of care, promotes effective communication, and supports ethical and legal compliance. Choosing the right template, customizing it to your specific needs, and adhering to best practices for writing effective notes are all crucial steps in maximizing its benefits. Ultimately, a well-maintained SOAP note is more than just a record; it’s a valuable resource for understanding the patient’s journey and delivering the best possible care.