Critical care environments demand meticulous documentation to ensure patient safety, continuity of care, and legal compliance. The sheer volume of data generated in an Intensive Care Unit (ICU) – vital signs, lab results, medication administration, interventions, and assessments – necessitates a structured and standardized approach. A well-designed ICU Report Template serves as that framework, streamlining the reporting process and minimizing the risk of errors or omissions. This article explores the essential components of an effective ICU report template, discusses different types of reports, and provides guidance on customizing templates to meet specific institutional needs.
The complexity of ICU care requires a reporting system that is both comprehensive and efficient. Without a standardized format, information can be fragmented, leading to miscommunication among healthcare providers and potentially impacting patient outcomes. A robust template ensures that all relevant data is captured consistently, facilitating accurate analysis and informed decision-making. Furthermore, standardized reporting is crucial for quality improvement initiatives, benchmarking performance, and meeting regulatory requirements.
The evolution of electronic health records (EHRs) has significantly impacted ICU reporting. While EHRs offer numerous advantages, including automated data collection and improved accessibility, the underlying report template remains a critical element. A poorly designed template within an EHR can negate many of its benefits, leading to frustration and inefficiencies. Therefore, careful consideration must be given to the design and implementation of these templates, ensuring they are user-friendly, clinically relevant, and adaptable to changing needs.
Ultimately, the goal of any ICU report is to provide a clear and concise summary of a patient’s condition and the care they have received. This requires a template that is not only comprehensive but also easy to understand and navigate. The following sections will delve into the key elements of a successful ICU Report Template and explore best practices for its development and utilization.
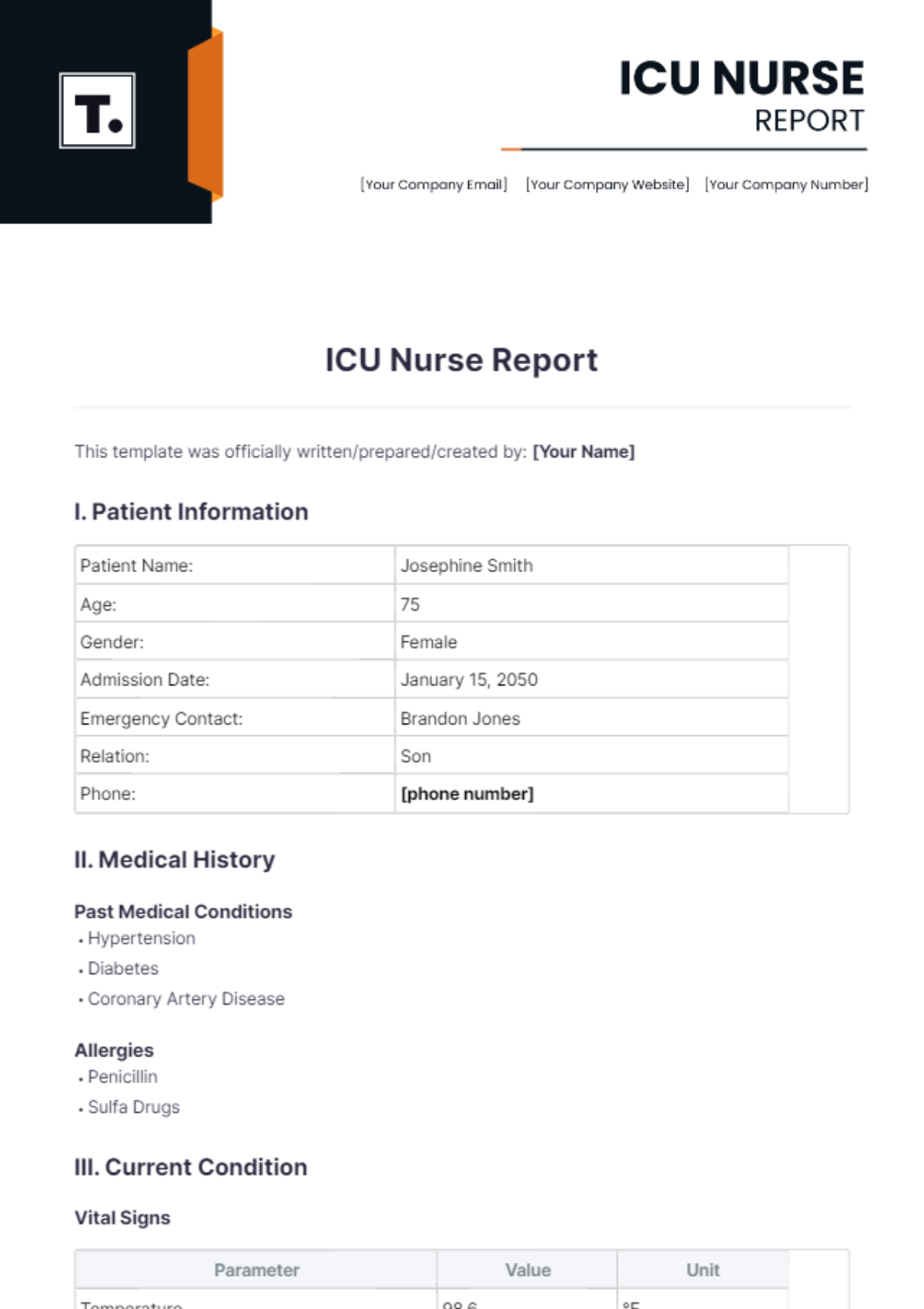
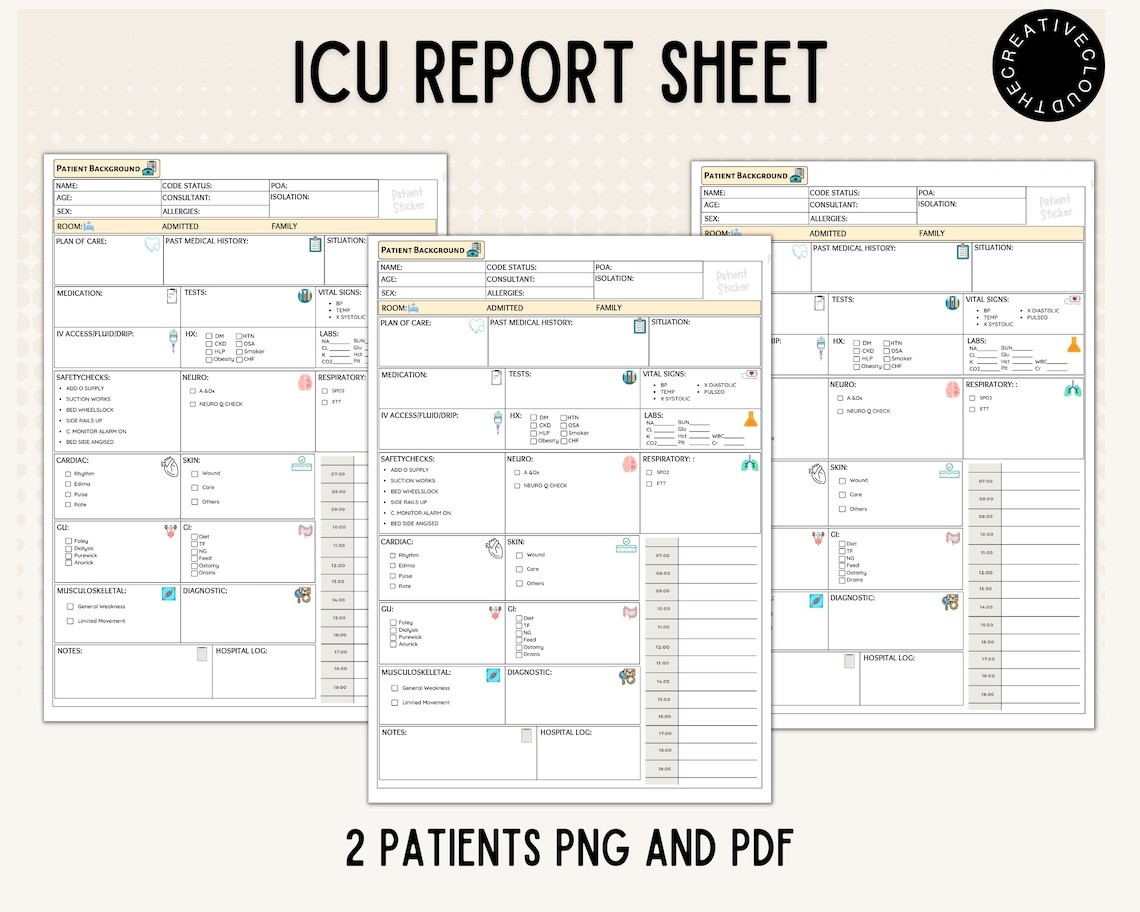
A comprehensive ICU report template should incorporate a variety of elements to capture the full scope of patient care. These elements can be broadly categorized into demographic information, medical history, current status, interventions, and future plans. The specific components included will vary depending on the type of report and the institution’s protocols.
This section should include basic patient details such as name, medical record number, date of birth, and attending physician. Accurate identification is paramount to avoid errors and ensure the correct patient record is being accessed.
A concise summary of the patient’s relevant medical history, including pre-existing conditions, allergies, and current medications, is essential. The presenting illness – the reason for the patient’s admission to the ICU – should also be clearly documented.
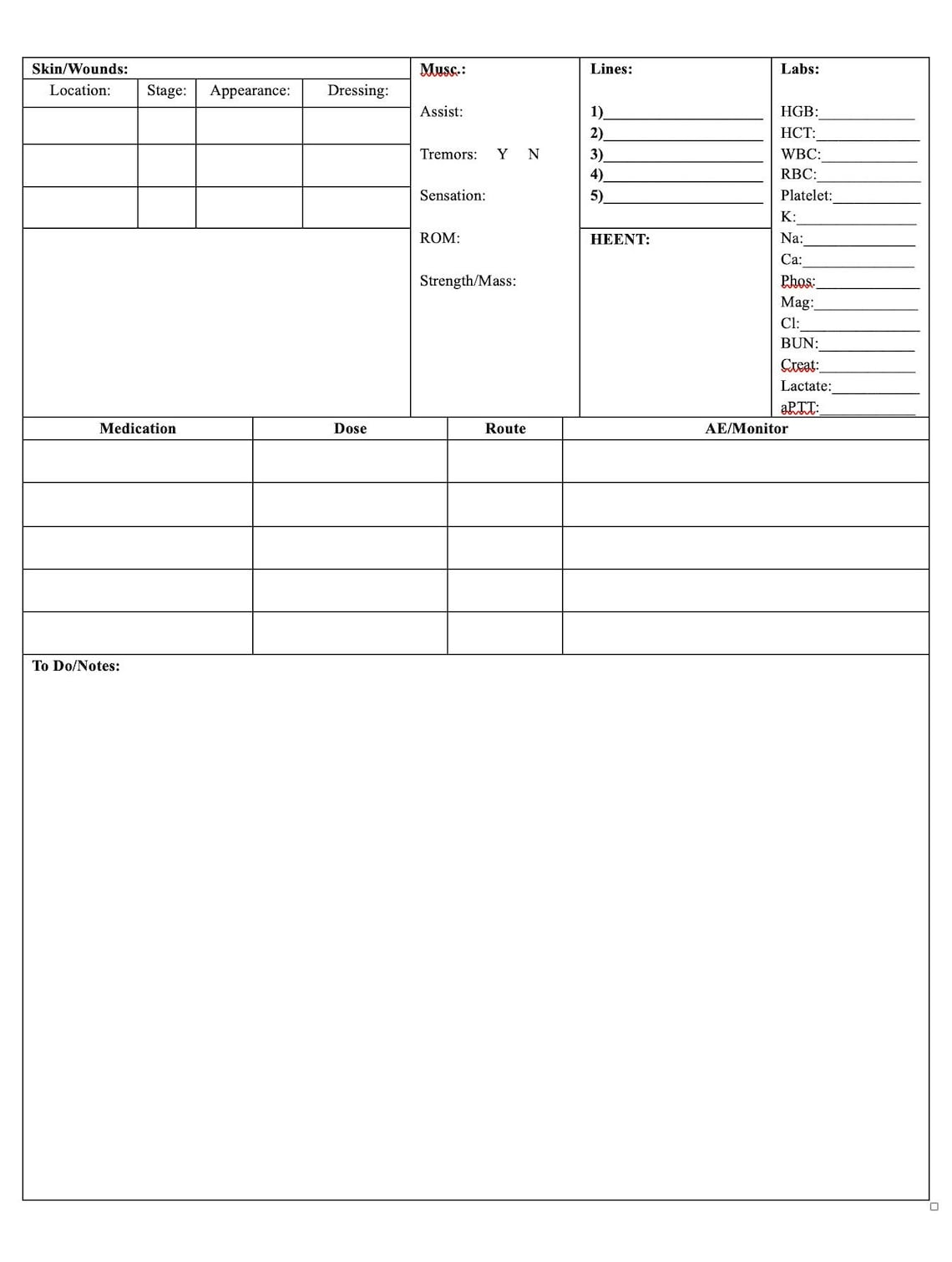
Continuous monitoring of vital signs is a hallmark of ICU care. The template should include sections for recording heart rate, blood pressure, respiratory rate, temperature, oxygen saturation, and other relevant physiological parameters. Trends in these values should be easily discernible.
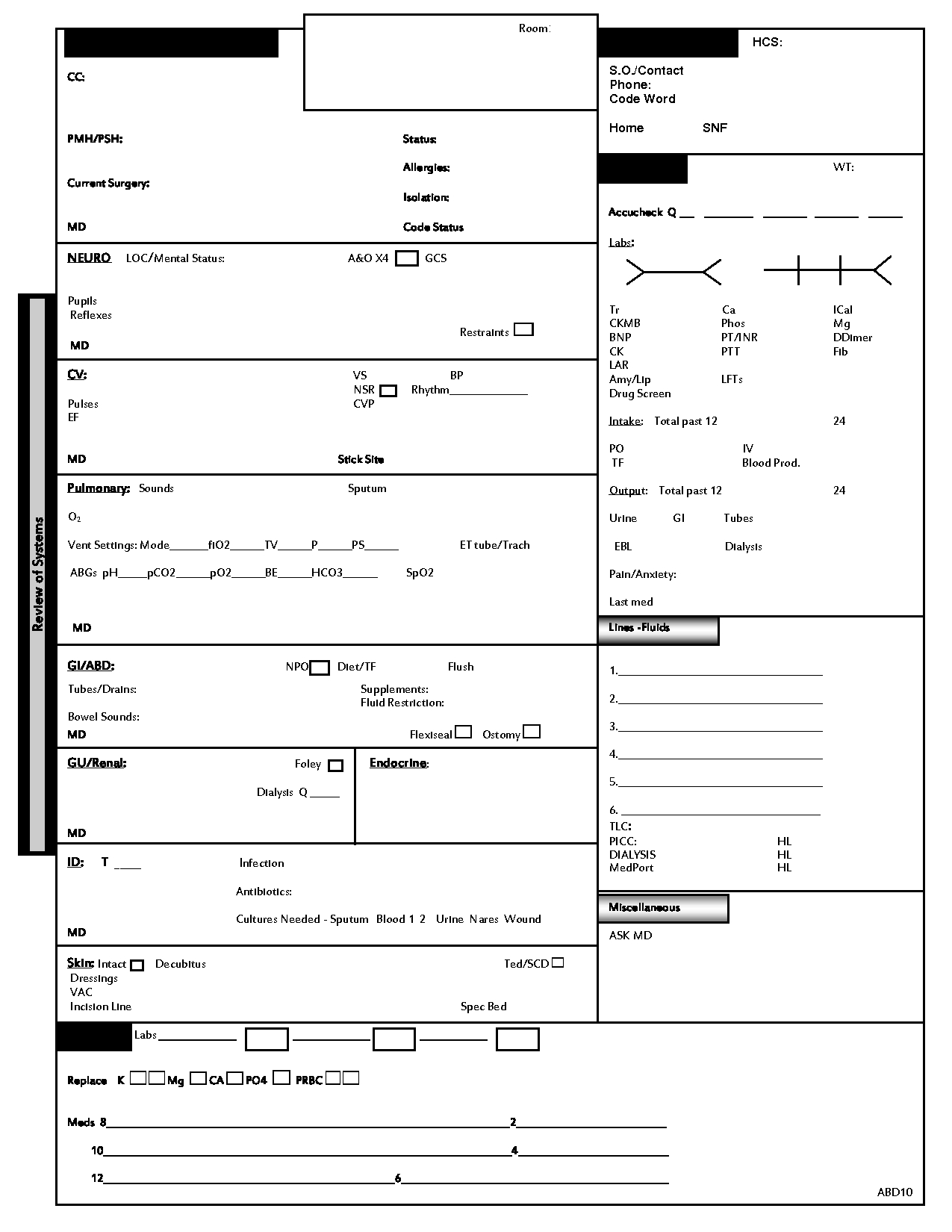
This section should document key laboratory findings (e.g., complete blood count, electrolytes, coagulation studies) and results of diagnostic imaging studies (e.g., chest X-ray, CT scan, MRI). Abnormal values should be clearly highlighted.
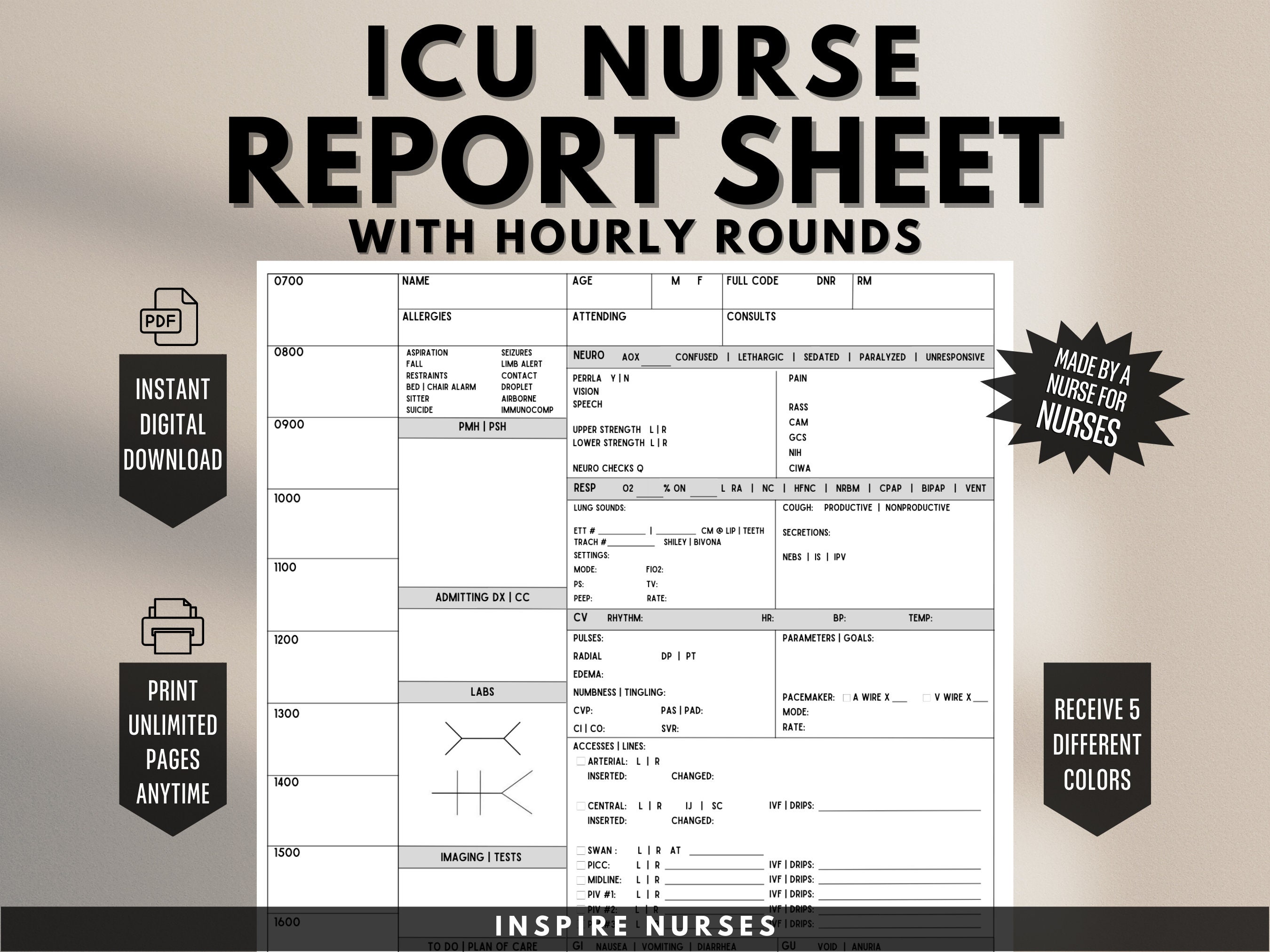
A detailed record of all medications administered, including dosage, route, and time of administration, is crucial. Fluid balance – including intake and output – should also be meticulously documented.
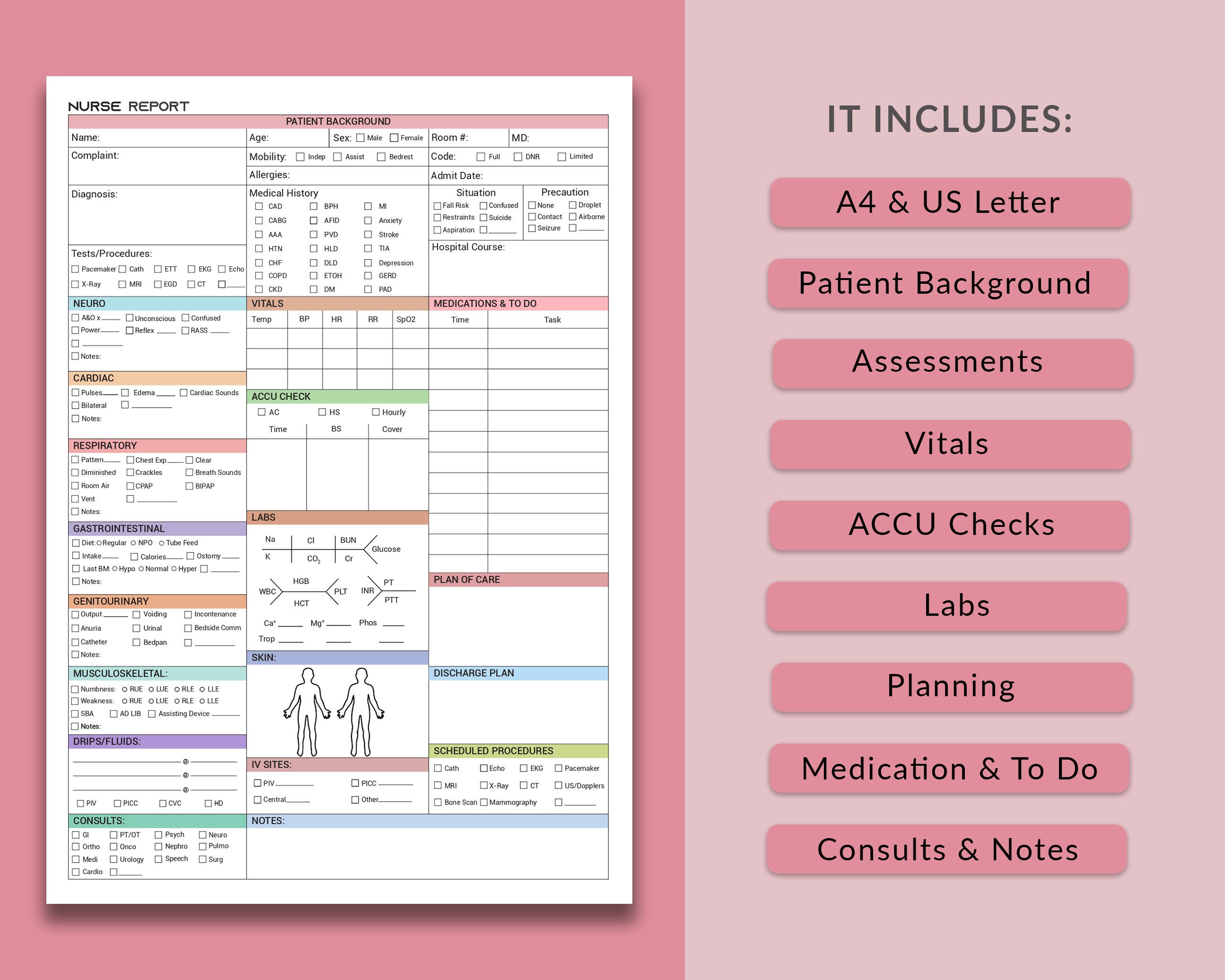
This section should document the findings of regular patient assessments, including neurological status, respiratory effort, and hemodynamic stability. All interventions performed, such as ventilator adjustments, medication administration, and procedures, should be clearly recorded.
The plan of care – outlining the goals for the patient’s treatment and the strategies for achieving those goals – should be clearly articulated. This section should also include any pending consultations or investigations.
Different types of ICU reports serve distinct purposes and may require different levels of detail. Understanding these distinctions is crucial for selecting the appropriate template.
These reports provide a comprehensive summary of the patient’s condition and progress over the preceding 24-hour period. They are typically used for communication among healthcare providers and for tracking the patient’s response to treatment.
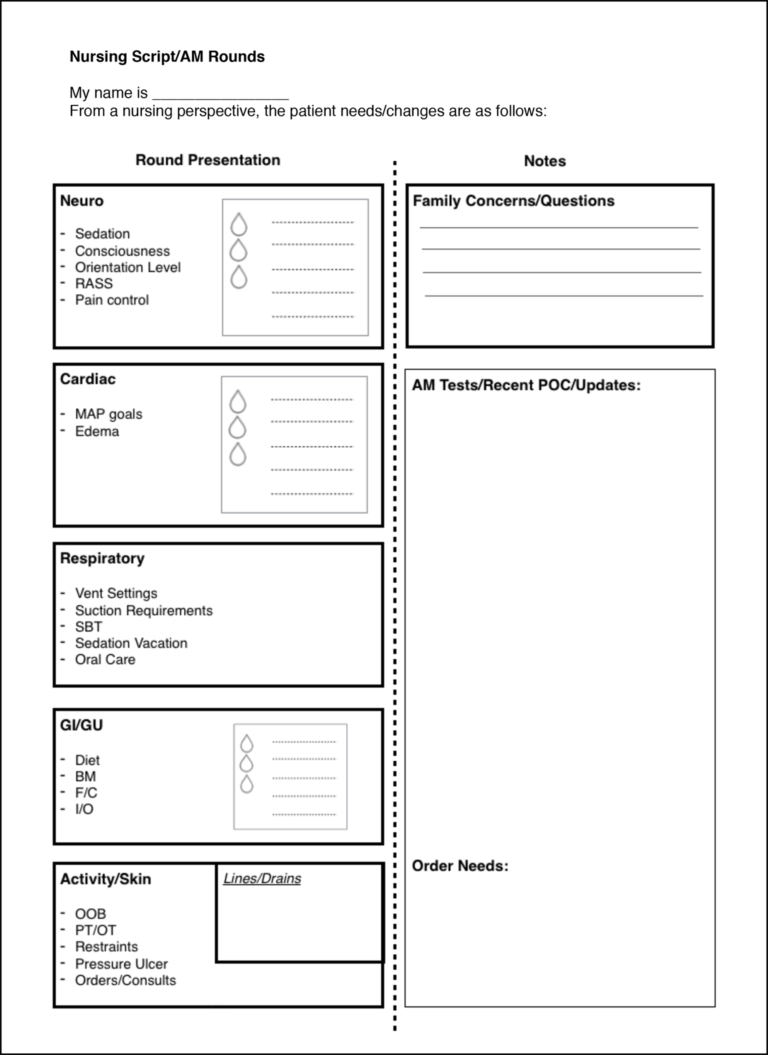
Shift reports are brief summaries of the patient’s condition and care plan, typically exchanged between nurses at the beginning and end of each shift. They focus on the most critical information needed to ensure continuity of care.
Transfer reports are used to communicate patient information to healthcare providers receiving the patient, either within the ICU or to another unit. They should include a concise summary of the patient’s medical history, current status, and plan of care.
Discharge summaries provide a comprehensive overview of the patient’s hospitalization, including the reason for admission, significant findings, treatments received, and discharge instructions.
Creating an effective ICU Report Template requires careful planning and consideration of the specific needs of the ICU.
The template should be easy to use and navigate, even under stressful conditions. Clear headings, logical organization, and intuitive data entry fields are essential.
The template should be customizable to accommodate different patient populations and clinical scenarios. The ability to add or remove fields, modify data entry formats, and incorporate institutional protocols is crucial.
The template should be seamlessly integrated with the EHR to ensure data accuracy and efficiency. Automated data collection and reporting capabilities can significantly reduce the workload for healthcare providers.
While customization is important, standardization is also key. Consistent use of terminology and data formats promotes clear communication and facilitates data analysis.
The template should be regularly reviewed and updated to reflect changes in clinical practice, technology, and regulatory requirements. Feedback from healthcare providers should be actively solicited and incorporated.
EHRs have revolutionized ICU reporting, offering numerous advantages over traditional paper-based systems.
EHRs can automatically collect data from bedside monitors and other devices, reducing the risk of manual errors and saving time for healthcare providers.
EHRs provide instant access to patient information from any location, facilitating communication and collaboration among healthcare providers.
EHRs enable the analysis of large datasets, allowing for the identification of trends and patterns that can inform quality improvement initiatives.
Most EHRs offer customizable reporting capabilities, allowing institutions to tailor ICU Report Template designs to meet their specific needs.
While EHRs offer many benefits, it’s crucial to ensure data integrity. Proper training and adherence to standardized protocols are essential to minimize errors and maintain data accuracy.
Successful implementation and maintenance of an ICU report template require a systematic approach.
Involve all relevant stakeholders – physicians, nurses, respiratory therapists, pharmacists, and IT staff – in the design and implementation process.
Provide comprehensive training to all users on how to use the template effectively.
Monitor the template’s performance and solicit feedback from users on a regular basis.
Conduct periodic audits to ensure data accuracy and compliance with institutional protocols.
Implement a version control system to track changes to the template and ensure that users are always using the most current version.
A well-designed and effectively utilized ICU Report Template is an indispensable tool for ensuring patient safety, promoting continuity of care, and facilitating quality improvement in the Intensive Care Unit. By incorporating the essential components outlined in this article, customizing templates to meet specific institutional needs, and leveraging the capabilities of electronic health records, healthcare organizations can optimize their reporting processes and enhance the quality of care provided to critically ill patients. Continuous evaluation and adaptation of these templates are vital to maintain their relevance and effectiveness in the ever-evolving landscape of critical care medicine.
