Effective patient care hinges on clear and accurate communication, and at the heart of this communication lie meticulously maintained nurse notes. These records are more than just documentation; they’re a vital tool for tracking patient progress, ensuring continuity of care, and providing a legal record of interventions and observations. A well-structured Nurse Notes Template helps standardize this process, promoting clarity and efficiency across nursing teams.
The importance of consistent and comprehensive nurse notes cannot be overstated. They facilitate seamless handoffs between shifts, allowing nurses to quickly understand a patient’s current status and needs. They also serve as a critical reference point for physicians and other healthcare professionals involved in the patient’s care, ensuring that everyone is working from the same understanding of the patient’s condition. Furthermore, accurate nurse notes are essential for legal protection, providing a detailed account of the care provided.
In the digital age, Nurse Notes Templates have evolved beyond paper charts to encompass electronic health records (EHRs). These digital templates offer numerous advantages, including improved legibility, easier accessibility, and the ability to incorporate structured data elements for enhanced analysis and reporting. Whether using paper or electronic formats, the principles of effective nurse note documentation remain the same: accuracy, clarity, conciseness, and completeness.
Ultimately, the goal of any Nurse Notes Template is to facilitate excellent patient care by providing a reliable and accessible record of nursing assessments, interventions, and patient responses. The information contained within these notes forms the foundation for informed decision-making and collaborative care planning, contributing significantly to positive patient outcomes. This article will explore the key components of an effective template and how it can be used to improve nursing documentation practices.

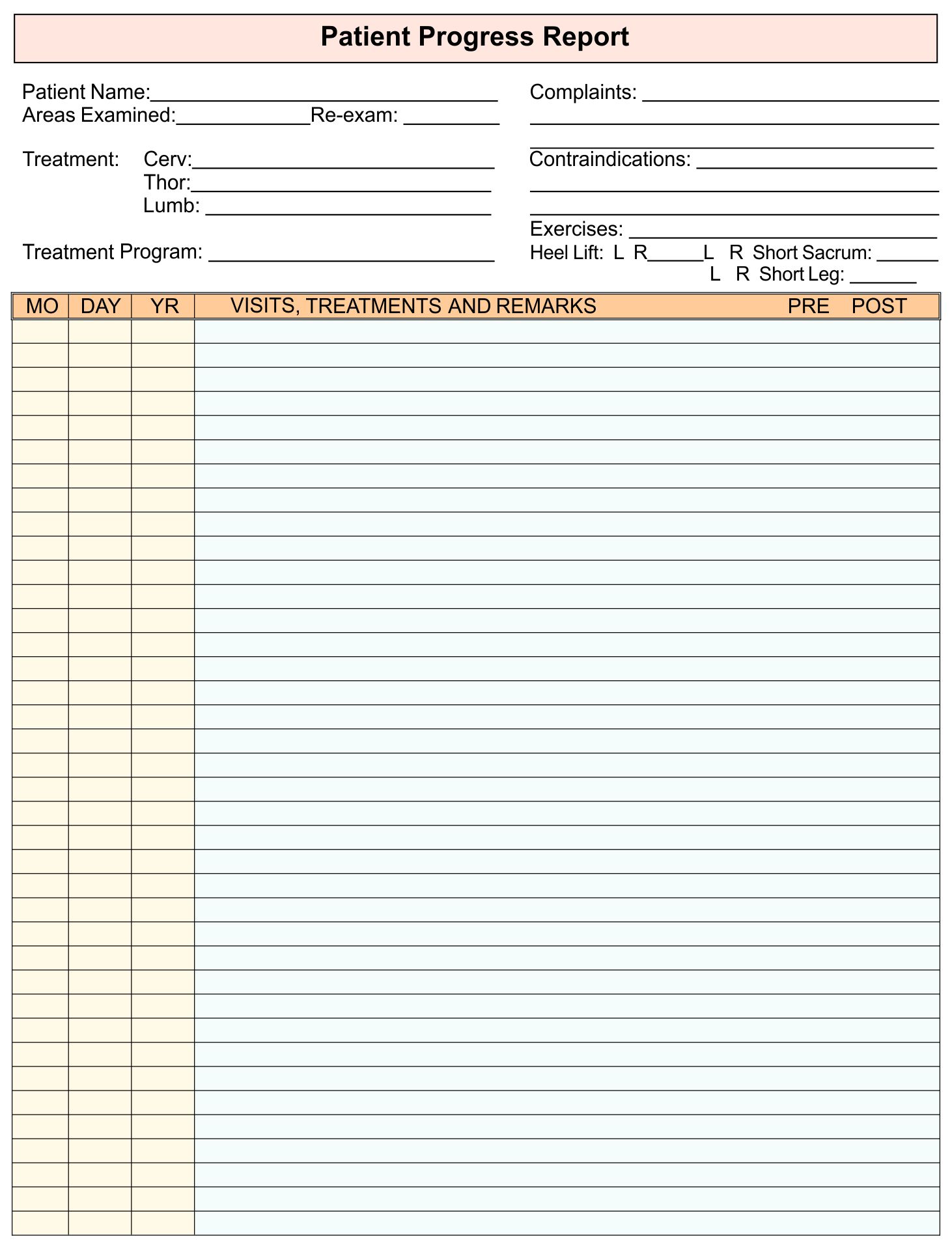
A well-designed Nurse Notes Template should include several essential components to ensure comprehensive and accurate documentation. These components cover various aspects of patient care, from initial assessments to ongoing monitoring and interventions. The specific elements may vary depending on the healthcare setting and patient population, but the underlying principles remain the same.
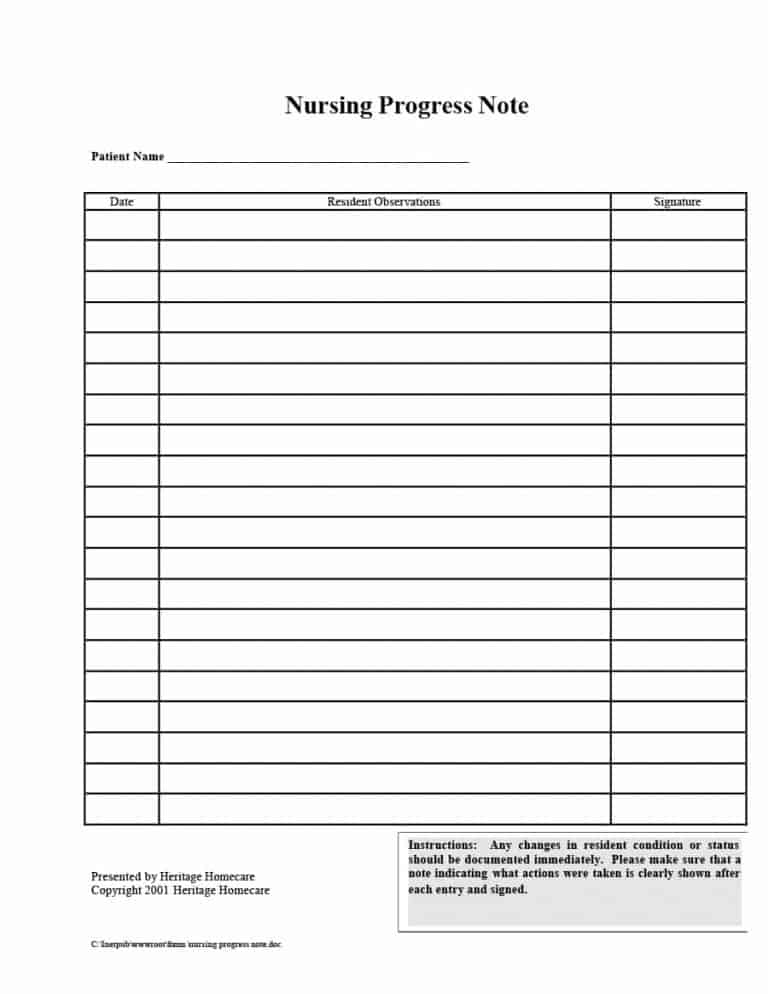
At the top of each note, clearly identify the patient using their full name, date of birth, medical record number, and any other relevant identifiers. This information ensures that the note is correctly associated with the intended patient and helps prevent errors.
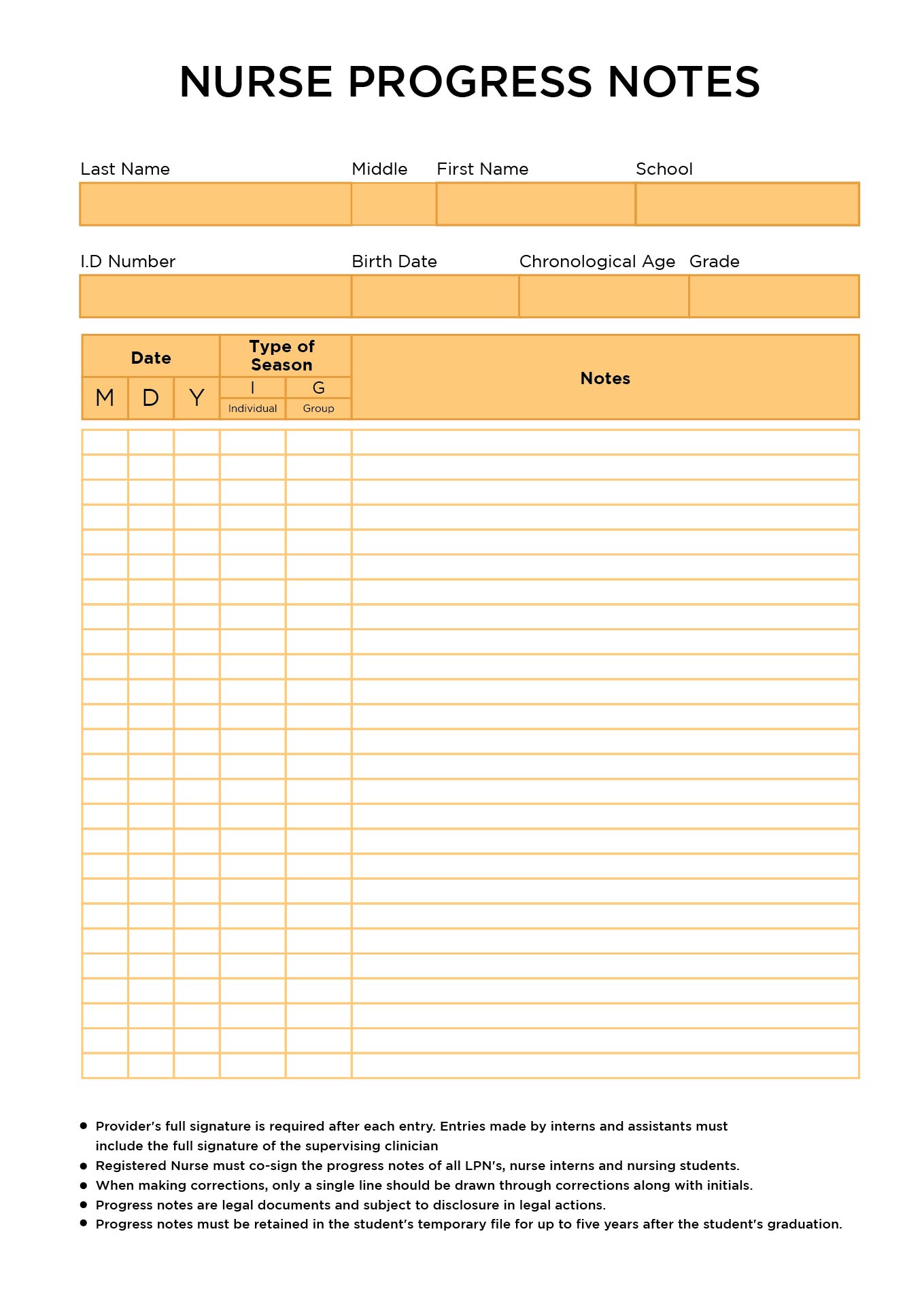
Each entry should be clearly dated and timed to establish a chronological record of events. The nurse making the entry should also sign or electronically authenticate the note to ensure accountability and identify the author.
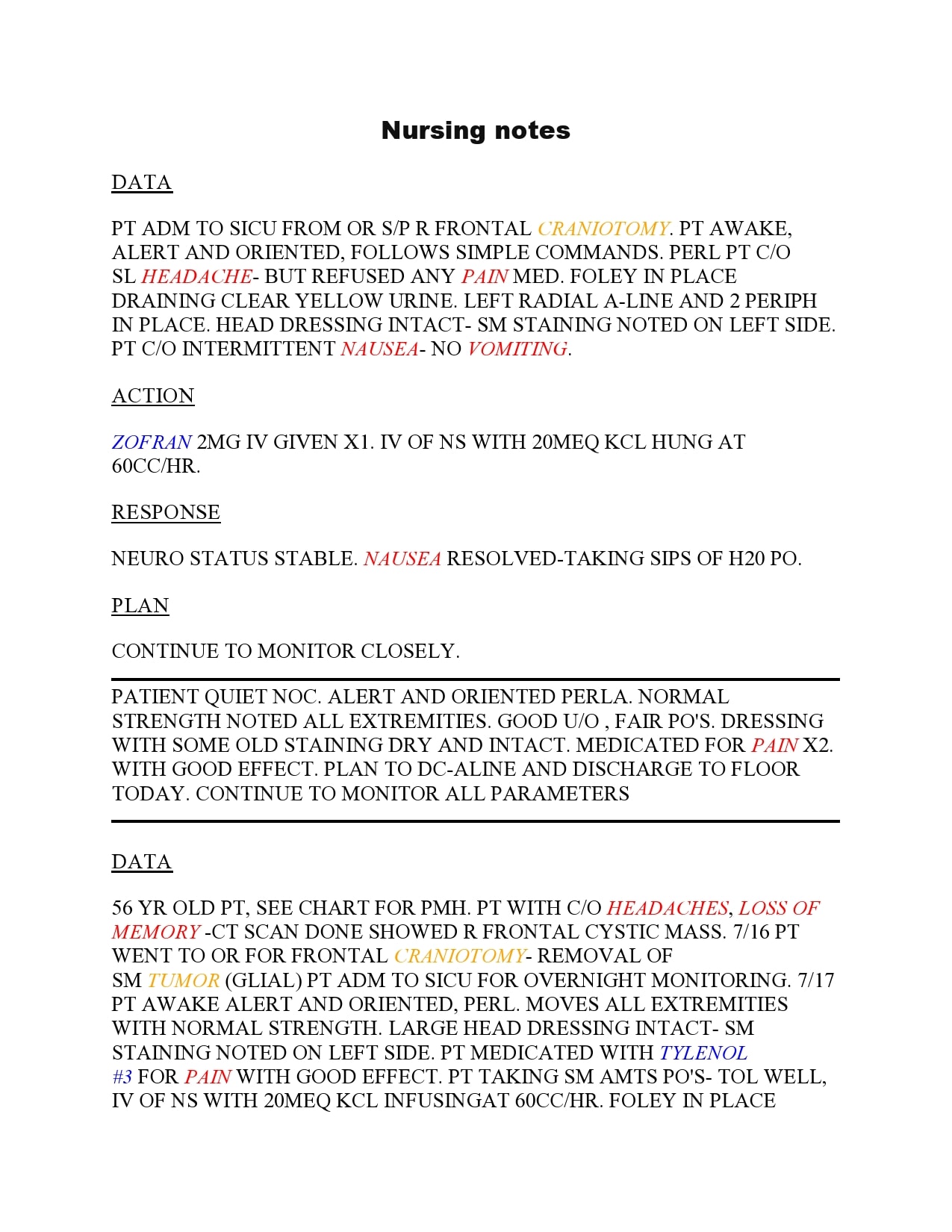
This section captures the patient’s perspective on their condition, including their symptoms, feelings, and concerns. Document the patient’s own words as accurately as possible, using quotation marks to indicate direct quotes. Examples include “Patient reports feeling nauseous” or “Patient states, ‘I have a throbbing headache.'”
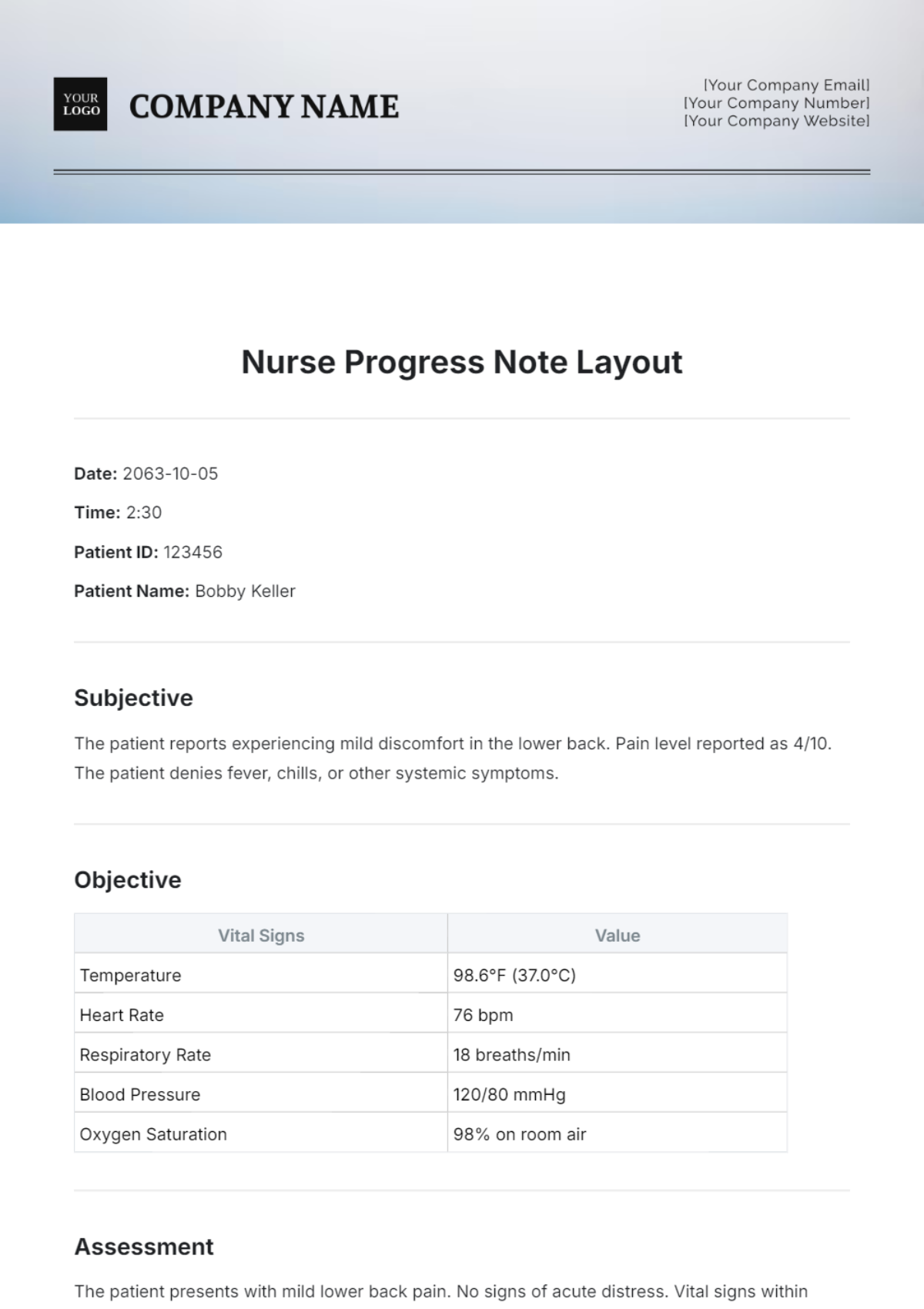
This section includes factual and measurable information obtained through observation, examination, and diagnostic testing. Include vital signs (temperature, pulse, respiration, blood pressure, oxygen saturation), physical assessment findings (e.g., lung sounds, skin condition), and laboratory results.

Based on the subjective and objective data, the nurse formulates an assessment of the patient’s condition. This section includes a summary of the patient’s current status, any identified problems or needs, and the nurse’s clinical judgment.
The plan outlines the nursing interventions that will be implemented to address the patient’s identified problems and needs. This section should be specific and measurable, including details such as medications administered, treatments performed, and patient education provided.

This section describes the actions taken by the nurse to implement the plan of care. Document the specific interventions performed, the patient’s response to these interventions, and any modifications made to the plan as a result.
This section evaluates the effectiveness of the nursing interventions in achieving the desired outcomes. Assess the patient’s progress toward goals and document any changes in their condition. This information is used to inform ongoing care planning and adjust interventions as needed.
Record any patient or family teaching that was performed, including the topics covered, the methods used, and the patient’s understanding of the information. This is particularly important for discharge planning and promoting self-management.
The specific type of Nurse Notes Template used will depend on the setting and the type of care being provided. Here are some common types of nurse notes:
These notes are completed upon a patient’s admission to a healthcare facility. They provide a comprehensive overview of the patient’s medical history, current condition, and initial assessment findings. They are essential for establishing a baseline and identifying any immediate needs or concerns.
Progress notes are used to document the patient’s ongoing progress throughout their hospital stay or treatment period. They track changes in the patient’s condition, the effectiveness of interventions, and any adjustments made to the plan of care. These notes are typically written at regular intervals, such as every shift or every day.
Discharge notes summarize the patient’s hospital stay or treatment period, including their final condition, medications, follow-up appointments, and any discharge instructions provided. They are crucial for ensuring a smooth transition to home or another care setting.
Focused notes address a specific problem or concern identified during the patient’s care. They provide a detailed account of the assessment, interventions, and evaluation related to that particular issue. These notes are often used to document changes in wound care, pain management, or other specific clinical areas.
Telephone notes document any phone conversations with patients, family members, or other healthcare providers. They include the date, time, and content of the conversation, as well as any actions taken as a result. These notes are important for maintaining a record of communication and ensuring continuity of care.
Implementing a standardized Nurse Notes Template offers numerous benefits for healthcare organizations and nursing staff.
A standardized template ensures that all nurses document patient information in a consistent and organized manner. This facilitates communication between nurses, physicians, and other healthcare providers, promoting a shared understanding of the patient’s condition and care plan.
A well-designed template streamlines the documentation process, allowing nurses to quickly and efficiently record patient information. This saves time and reduces the risk of errors or omissions.
Standardized templates help to minimize errors by providing a structured format for documenting patient information. This reduces the likelihood of missing important details or misinterpreting information.
Consistent documentation ensures that all members of the healthcare team have access to the same information about the patient’s condition and care plan. This promotes continuity of care and reduces the risk of fragmented or uncoordinated care.
Accurate and complete nurse notes provide a legal record of the care provided to the patient. This can be crucial in the event of a lawsuit or other legal action.
Standardized data collection within a Nurse Notes Template allows for easier data analysis and reporting. This can be used to identify trends, improve patient outcomes, and inform quality improvement initiatives.
While using a template is helpful, following best practices for documentation is crucial for creating effective and useful nurse notes.
Record information accurately and objectively, avoiding subjective opinions or judgments. Base your notes on facts and observations, not assumptions or interpretations.
Use clear and concise language, avoiding jargon or abbreviations that may not be understood by all readers. Get straight to the point without unnecessary details.
Document all relevant information, including subjective and objective data, assessments, plans, interventions, and evaluations. Do not omit important details or leave gaps in the record.
Document information as soon as possible after it occurs, while the details are still fresh in your mind. Avoid delaying documentation, as this can lead to errors or omissions.
Ensure that your notes are free of grammatical errors and spelling mistakes. This enhances clarity and credibility.
Adhere to HIPAA regulations and protect patient privacy by avoiding the inclusion of unnecessary personal information in your notes. Only include information that is relevant to the patient’s care.
While standardized templates offer many benefits, it’s important to customize them to meet the specific needs of your healthcare setting and patient population.
A template designed for a medical-surgical unit will differ from one designed for a pediatric or psychiatric setting. Tailor your template to reflect the unique aspects of your specialty.
Include assessment elements that are relevant to the types of patients you typically care for. For example, a cardiac unit template might include specific assessments of heart sounds, edema, and chest pain.
If you frequently encounter certain types of problems or conditions, consider adding dedicated sections to your template for documenting information related to those issues.
Periodically review and revise your template to ensure that it remains relevant and effective. Solicit feedback from nursing staff and other stakeholders to identify areas for improvement.
Electronic Health Records (EHRs) have revolutionized nursing documentation, offering numerous advantages over traditional paper charts. EHRs integrate Nurse Notes Templates seamlessly, enhancing efficiency, accuracy, and accessibility.
EHRs often incorporate structured data entry elements, such as drop-down menus, checkboxes, and standardized codes. This simplifies the documentation process and ensures consistency in data collection.
EHRs can provide automated prompts and reminders to guide nurses through the documentation process and ensure that all required information is captured.
EHRs integrate with other healthcare systems, such as laboratory, radiology, and pharmacy systems. This allows nurses to access relevant patient information quickly and easily, improving care coordination.
EHRs eliminate the problem of illegible handwriting, ensuring that all members of the healthcare team can easily read and understand the information contained in the nurse notes.
EHRs offer enhanced security features to protect patient privacy and confidentiality. Access to patient information is controlled through user IDs and passwords, and audit trails track all activity within the system.
Different specialties might require specific information to be included in their note templates. Here are some examples:
The Nurse Notes Template is a cornerstone of effective patient care, facilitating clear communication, ensuring continuity of care, and providing a legal record of nursing interventions. By understanding the key components of an effective template, different types of nurse notes, and the benefits of standardization, nurses can improve their documentation practices and contribute to positive patient outcomes. Whether using paper charts or electronic health records, the principles of accuracy, clarity, conciseness, and completeness remain paramount. Regularly reviewing and customizing templates, along with ongoing education and training, will ensure that nurse notes remain a valuable tool for delivering high-quality, patient-centered care.