Effective communication is the bedrock of safe patient care, and within the fast-paced environment of healthcare, the nursing handoff is arguably one of the most critical processes. A poorly executed handoff can lead to medication errors, delayed treatments, and, tragically, adverse patient outcomes. To mitigate these risks and ensure a seamless transition of patient responsibility, healthcare facilities rely heavily on standardized documentation – specifically, a well-constructed Nursing Handoff Report Template. This document serves as a centralized record, capturing vital information about a patient’s condition, treatment plan, and any pertinent observations. It’s more than just a formality; it’s a safeguard, a tool for continuity of care, and a legal record.
The importance of a robust handoff process extends beyond simply transferring information. It fosters collaboration between nurses, physicians, and other healthcare professionals, promoting a shared understanding of the patient’s needs. A comprehensive report allows the receiving team to quickly assess the patient’s status, identify potential risks, and implement the appropriate care plan. Furthermore, it provides a valuable audit trail, documenting the care provided and facilitating accountability. Investing in a reliable and adaptable Nursing Handoff Report Template is therefore a strategic investment in patient safety and operational efficiency.
Creating a truly effective template requires careful consideration of the information that needs to be conveyed. It’s not enough to simply list basic data points; the template should be designed to capture the nuances of the patient’s condition and the rationale behind the care plan. The goal is to provide the receiving nurse with a complete picture, enabling them to confidently assume responsibility for the patient’s well-being. This article will delve into the essential components of a successful template, exploring best practices and offering guidance on tailoring it to specific healthcare settings.

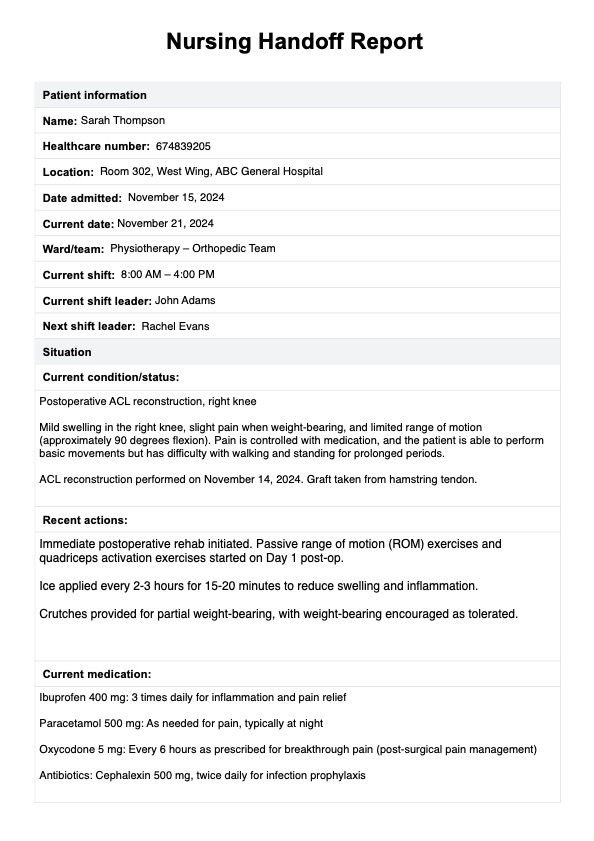
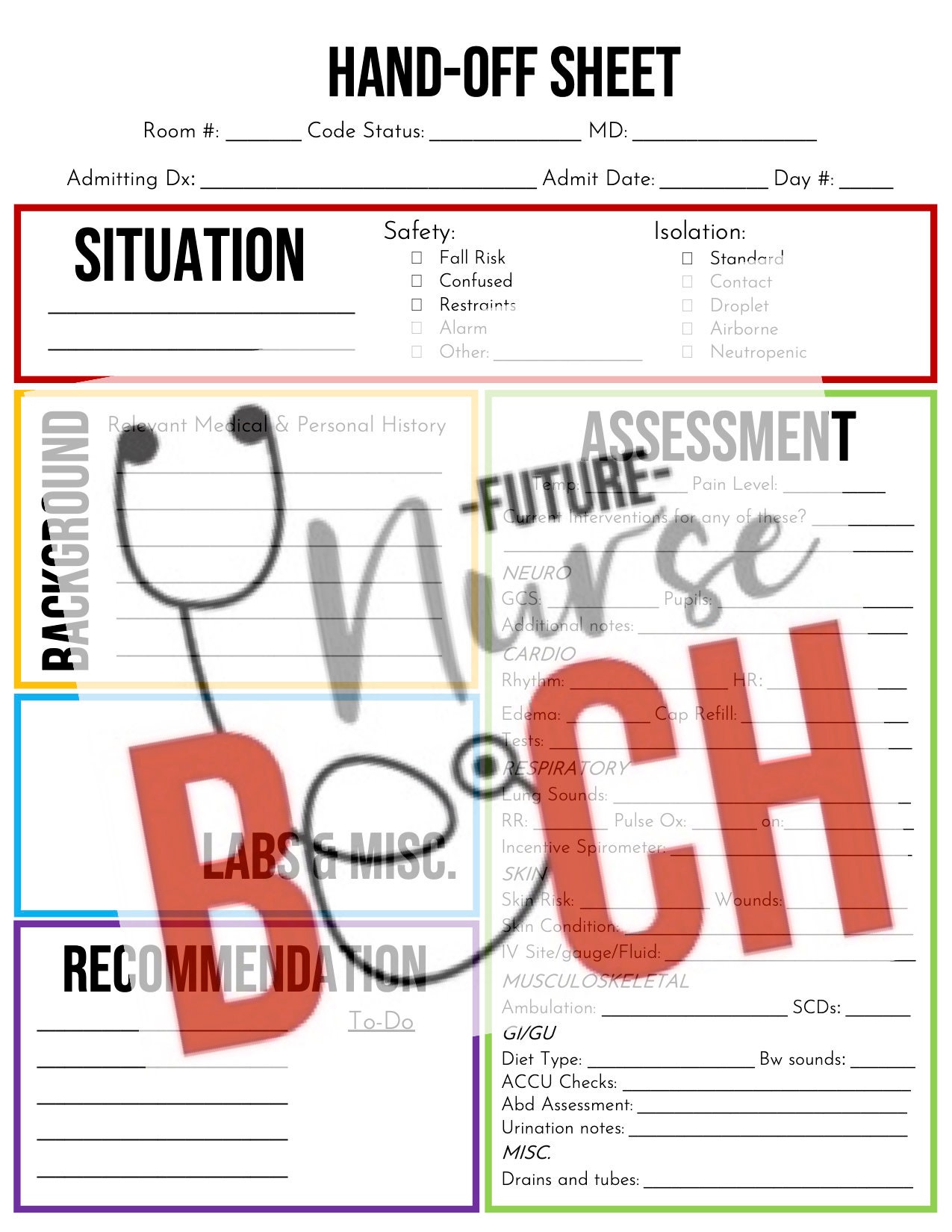
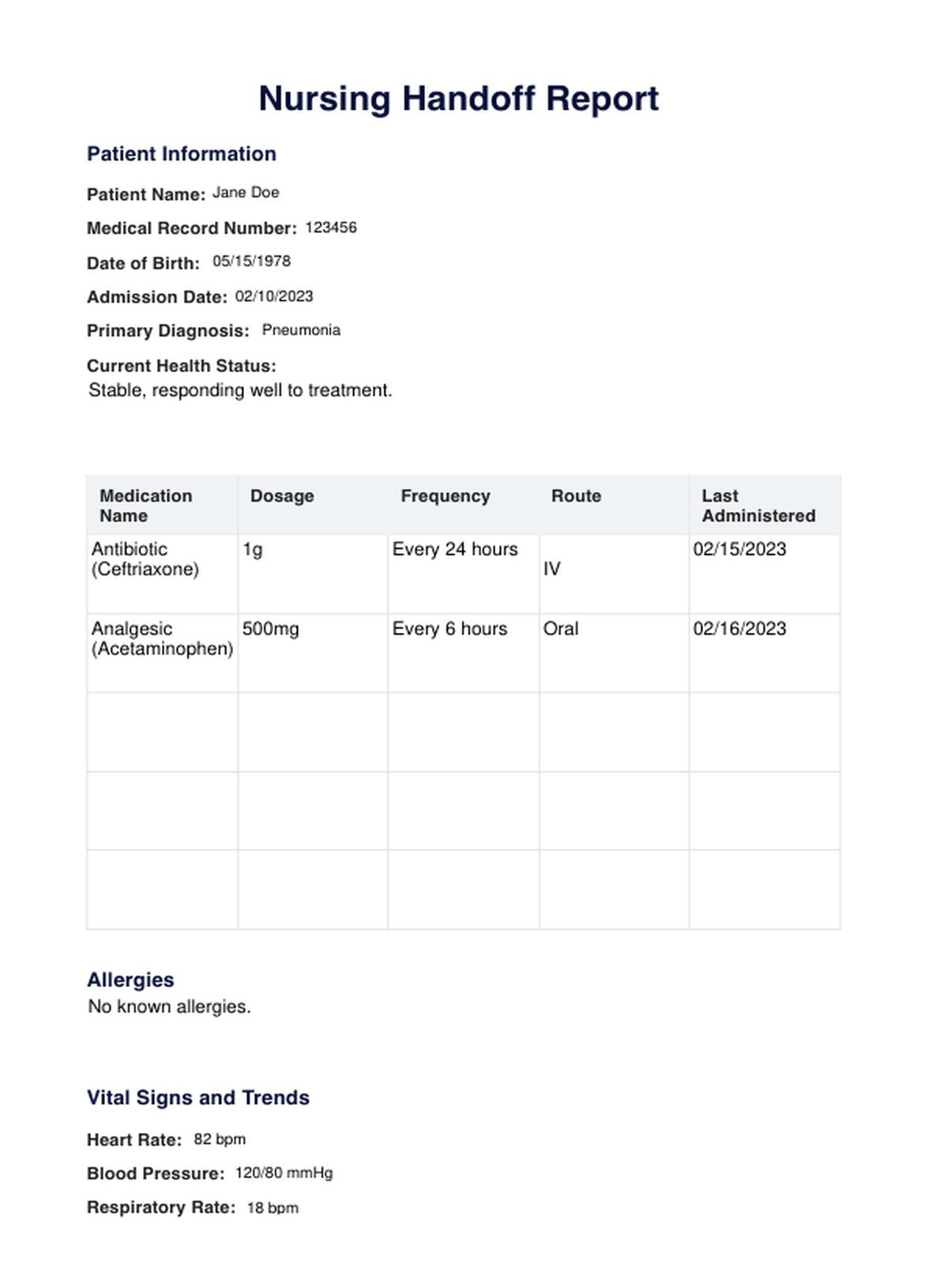
A well-designed Nursing Handoff Report Template should include several key sections to ensure comprehensive information transfer. These sections aren’t mutually exclusive; often, information will overlap and require concise summarization.
This section is the foundation of the report and must be meticulously accurate. It includes:

Clearly articulate the patient’s primary reason for seeking care and their current state. Use objective language, avoiding subjective interpretations. Include:
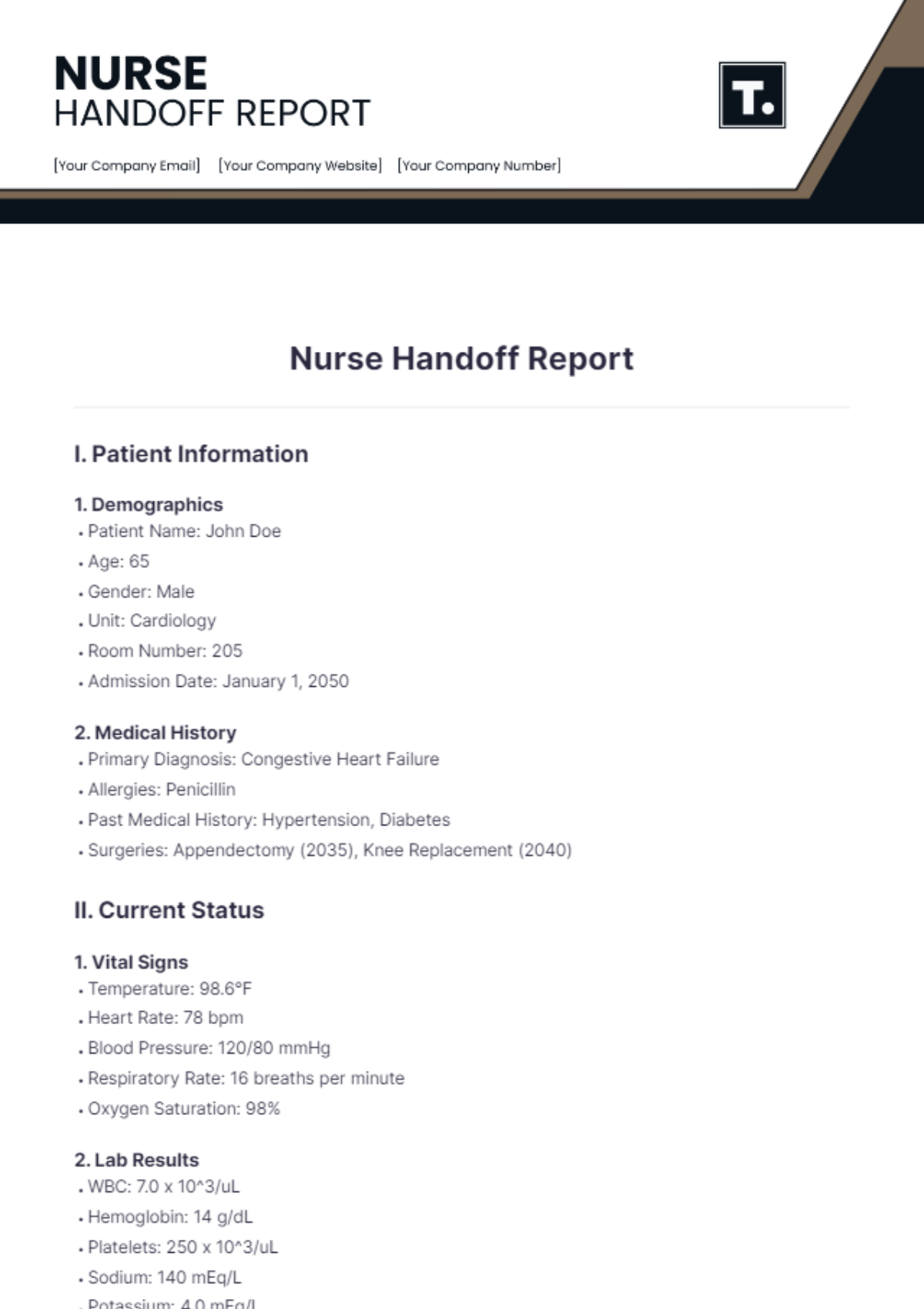
This section details the nurse’s observations and assessment results. It’s crucial to document:
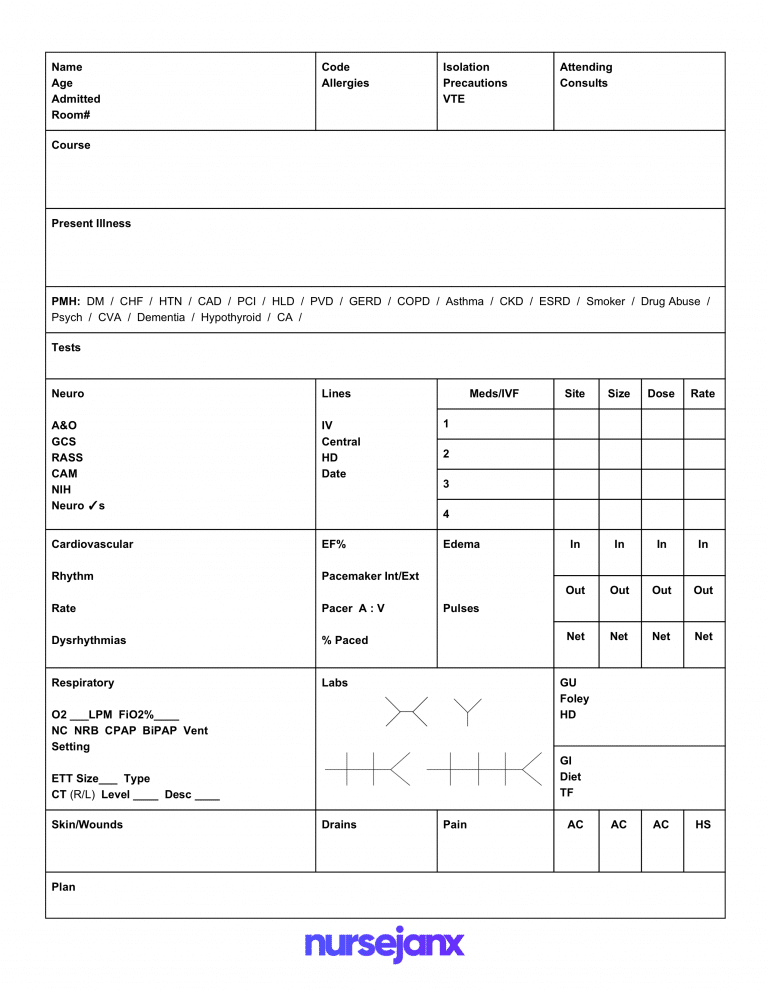
Outline the current care plan, including:
Document any concerns raised by the patient or their family, as well as any specific requests they may have. This demonstrates a focus on patient-centered care.
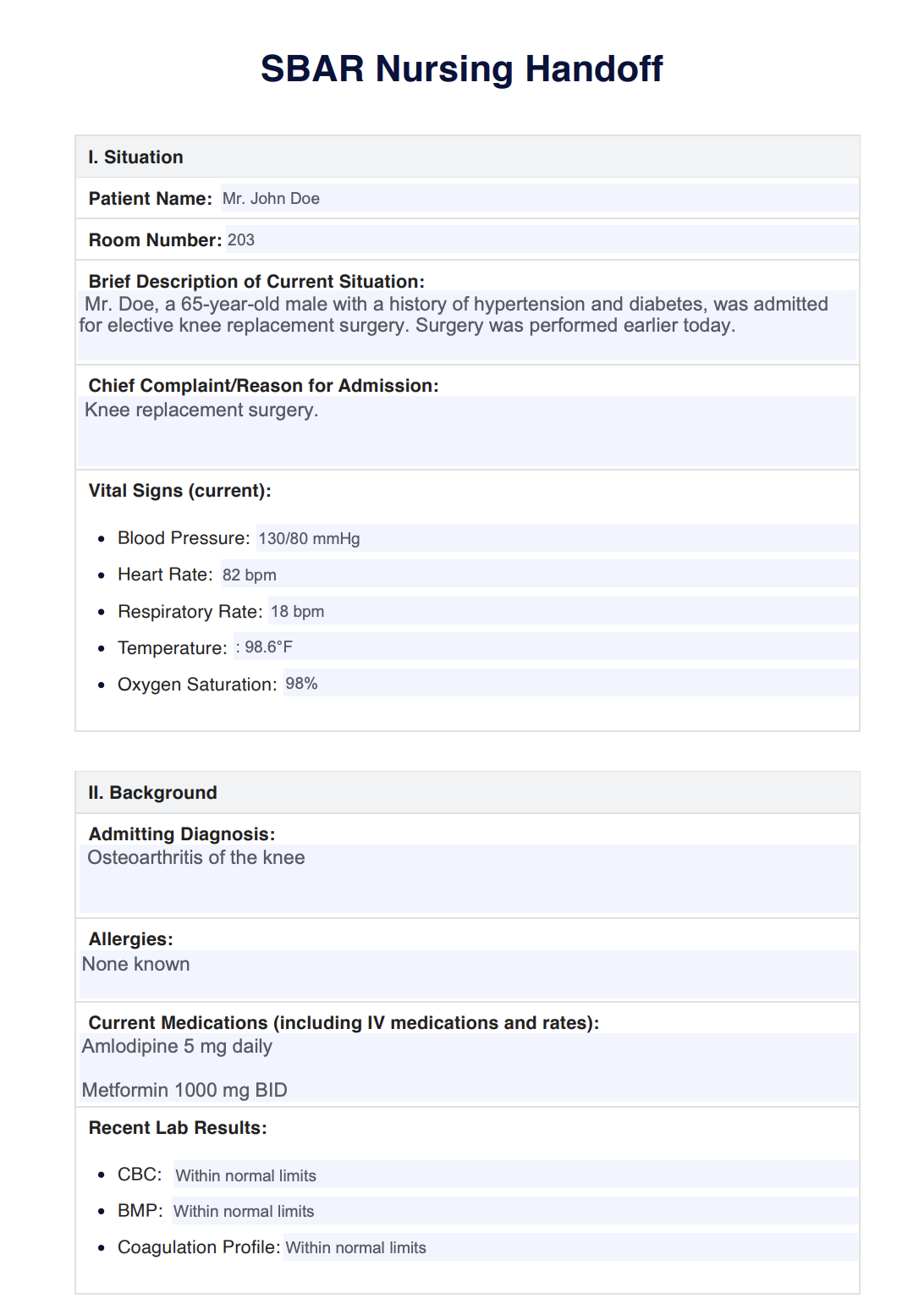
Clearly state the plan for the incoming nurse, including:
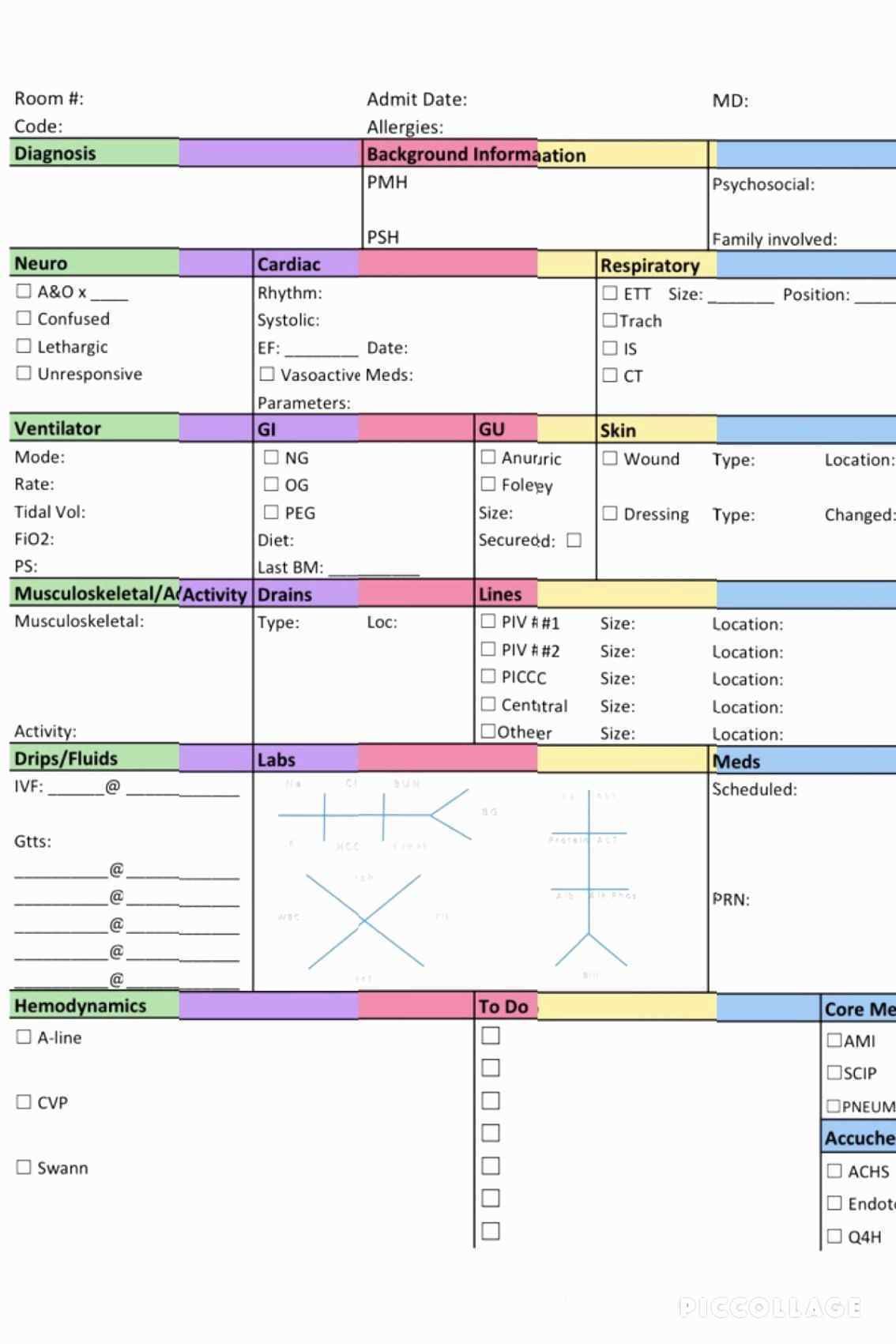
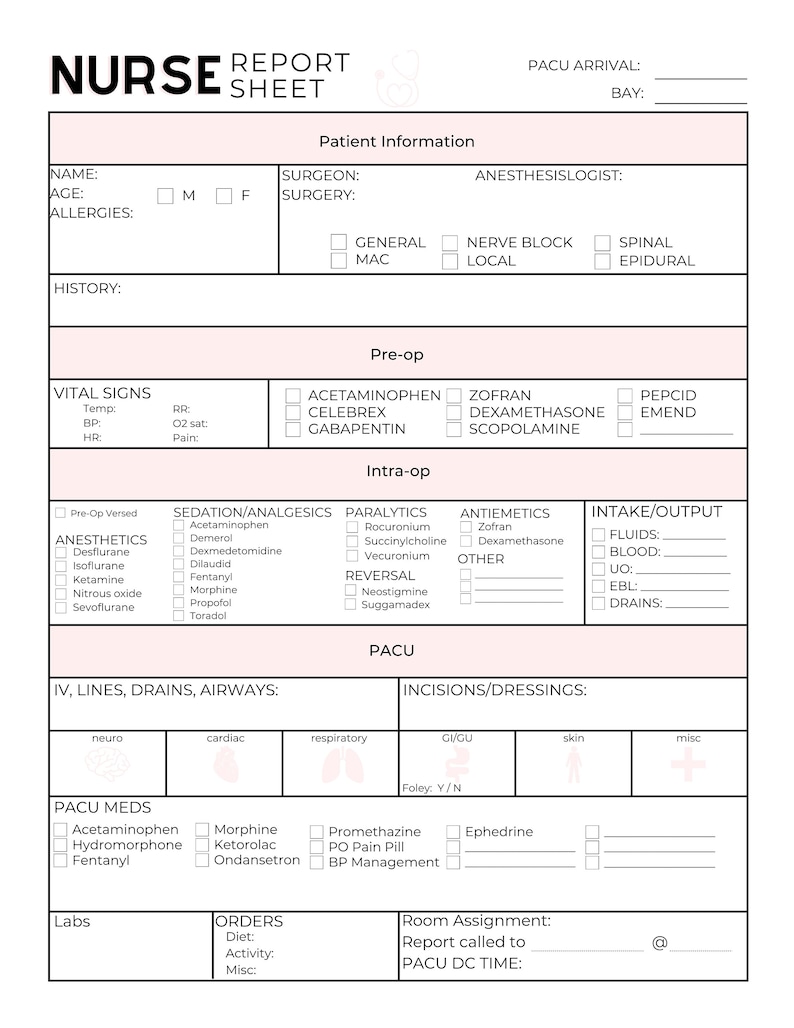
While the core components remain consistent, Nursing Handoff Report Templates can vary depending on the healthcare setting and the specific needs of the patient population.
Many hospitals and healthcare systems utilize standardized templates, often electronic, to ensure consistency and facilitate data analysis. These templates are typically pre-populated with common fields and may include drop-down menus and checkboxes to streamline the documentation process.
Some organizations opt for customizable templates that allow for greater flexibility and the ability to tailor the report to individual patient needs. This approach can be particularly useful in specialized areas of care, such as critical care or oncology.
In some settings, a simple shift change log is used, focusing on key changes in the patient’s condition and care plan. While less detailed than a full report, it still provides a valuable record of information transfer.
Increasingly, Nursing Handoff Report Templates are integrated directly into the EHR, allowing for seamless data transfer and reducing the risk of errors. EHR-based handoffs often include features such as automated alerts and reminders.
Simply filling out a template isn’t enough; the information must be accurate, complete, and communicated effectively.
Complete the report as soon as possible after the shift change, while the information is still fresh in your mind.
Use clear, concise language, avoiding jargon and abbreviations that may not be understood by the receiving nurse.
Document observations objectively, avoiding subjective interpretations or opinions.
Double-check all information for accuracy, including vital signs, medication dosages, and patient allergies.
Verbal communication is just as important as written documentation. Discuss the key points of the report with the receiving nurse to ensure a thorough understanding.
Always include your signature and the current timestamp to verify the authenticity of the report.
Technology plays a crucial role in enhancing the efficiency and effectiveness of Nursing Handoff Report Templates.
These systems streamline the handoff process by providing a centralized platform for documenting and sharing information. They often include features such as automated alerts, real-time updates, and secure messaging.
Mobile apps allow nurses to complete handoff reports on the go, using tablets or smartphones. This is particularly useful in busy hospital environments.
Voice-to-text technology can be used to dictate handoff reports, reducing the time and effort required for documentation.
Proper documentation is essential for legal and regulatory compliance.
All handoff reports must be handled in accordance with HIPAA regulations, ensuring patient privacy and confidentiality.
Accurate and complete handoff reports can help mitigate the risk of medical errors and adverse patient outcomes.
Healthcare facilities should regularly audit handoff reports to ensure compliance with established protocols.
A well-designed and consistently utilized Nursing Handoff Report Template is an indispensable tool for ensuring patient safety and promoting effective communication within the healthcare team. By incorporating the key components outlined in this article and embracing best practices, healthcare organizations can significantly reduce the risk of errors and improve the overall quality of patient care. Investing in robust handoff processes, including the appropriate template and supporting technology, demonstrates a commitment to patient-centered care and operational excellence. Continual evaluation and refinement of the template, alongside ongoing training for nursing staff, are vital to maintaining its effectiveness and adapting to evolving healthcare needs. Ultimately, a seamless and informative handoff is a cornerstone of a safe and reliable healthcare system.