The creation of thorough and accurate medical documentation is paramount in healthcare, and the operative note stands as a critical component of a patient’s health record. This document details the surgical procedure performed, providing a comprehensive account for continuity of care, billing purposes, and potential legal considerations. A well-structured operative note template can significantly streamline this process, ensuring all essential information is captured consistently and efficiently. It’s not merely a formality; it’s a vital communication tool between surgeons, anesthesiologists, nurses, and other healthcare professionals involved in the patient’s care.
Surgical documentation has evolved over time, moving from handwritten notes to electronic health record (EHR) systems. While EHRs offer numerous advantages, they also present challenges in maintaining clarity and conciseness. Utilizing a standardized template helps mitigate these issues, promoting uniformity and reducing the risk of omissions. A good template acts as a checklist, prompting the surgeon to include all necessary details, ultimately improving the quality and reliability of the operative record.

The importance of a detailed operative note extends beyond immediate patient care. It serves as a historical reference for future treatments, aids in research and quality improvement initiatives, and can be crucial in the event of a medical-legal dispute. Therefore, investing time in developing or selecting a robust operative note template is a worthwhile endeavor for any surgical practice.

Finally, remember that operative notes are often reviewed by coders for billing accuracy. A complete and well-organized note facilitates accurate coding, maximizing reimbursement and minimizing audit risks.
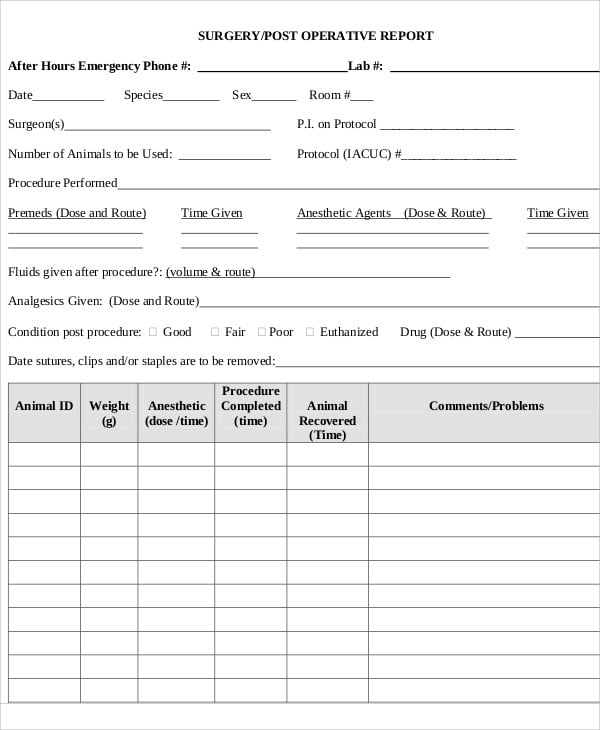
An operative note isn’t simply a narrative of what happened in the operating room. It’s a structured document with specific sections designed to convey critical information. Understanding these components is essential for both creating and utilizing an operative note template effectively.
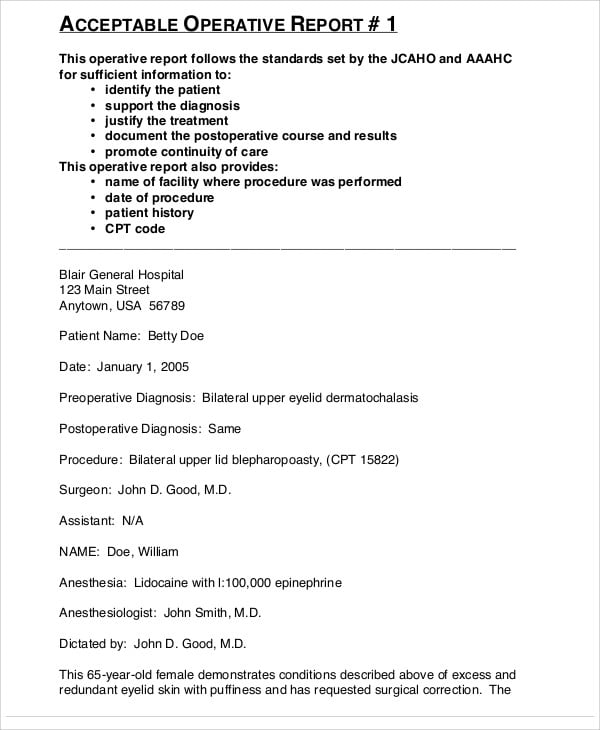
This section clearly states the patient’s diagnosis before the surgery. It should be specific and include relevant details, such as the stage of a cancer or the type of fracture. This provides context for the surgical intervention.
This section details the final diagnosis after the surgery. It may be the same as the preoperative diagnosis, but often it’s refined based on intraoperative findings. For example, a suspected appendicitis might be confirmed as a perforated appendix with peritonitis.

Clearly identify the primary surgeon and all assisting surgeons. This establishes accountability and clarifies roles during the procedure. Include the names and credentials of all personnel involved.
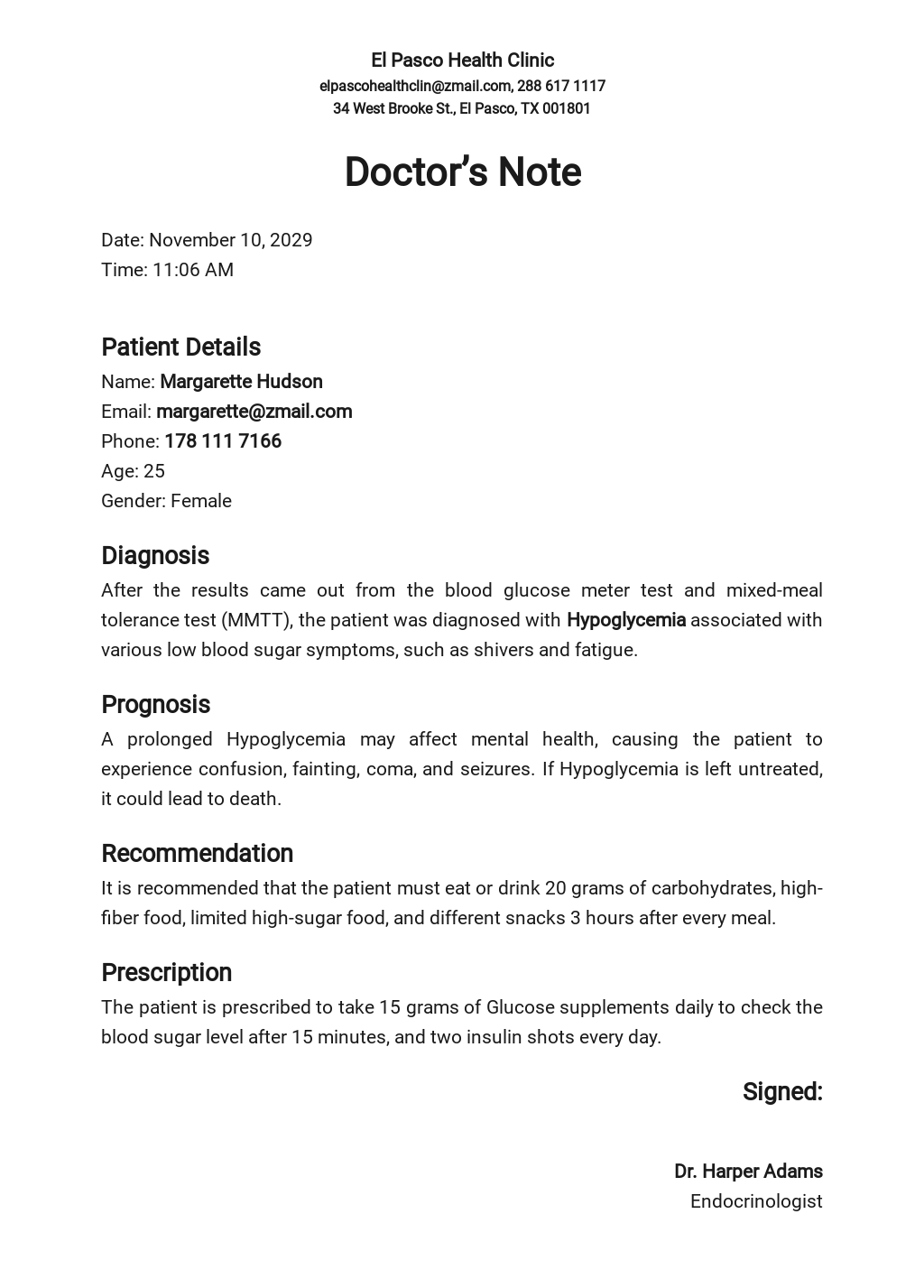
Specify the type of anesthesia used (e.g., general, regional, local) and the anesthesiologist’s name. Note any significant anesthetic events or complications.
This is the core of the operative note. It provides a detailed, step-by-step account of the surgical procedure performed. This section should be written in a chronological order and include:
If any implants were used during the surgery (e.g., screws, plates, prostheses), document the type, size, and serial number of each implant.
Accurately estimate the amount of blood lost during the surgery. This is important for assessing the patient’s hemodynamic stability and for billing purposes.
Document any complications that occurred during the surgery, no matter how minor. This includes things like bleeding, nerve injury, or instrument malfunction.
If any tissue specimens were sent to pathology, document the type of specimen and the location from which it was obtained.
While many pre-made templates are available, tailoring one to your specific specialty and practice can improve efficiency and ensure all relevant information is captured. Here’s a guide to designing your own operative note template.
Most EHR systems allow you to customize templates. Leverage these features to create a template that aligns with your workflow. Consider using drop-down menus and checkboxes to streamline data entry.
Different surgical specialties require different levels of detail in the operative note. For example, a neurosurgical operative note will likely focus on detailed neurological findings and anatomical landmarks, while an orthopedic operative note will emphasize implant details and fracture reduction techniques.
Integrate checklists into your template to ensure that all essential elements are addressed. This can help prevent omissions and improve the completeness of the operative note.
While thoroughness is important, strive for clarity and conciseness. Avoid jargon and use precise language. A well-written operative note should be easy to understand by all members of the healthcare team.
Implementing a standardized operative note template offers numerous benefits for surgeons, healthcare facilities, and patients.
A template acts as a reminder, prompting surgeons to include all necessary information. This reduces the risk of errors and omissions.
A standardized format facilitates clear communication between healthcare professionals.
A complete and well-organized operative note simplifies the billing and coding process, maximizing reimbursement.
Thorough documentation provides a strong defense in the event of a medical-legal dispute.
A template streamlines the documentation process, saving time and effort.
The debate between electronic and paper-based templates continues, but the trend is clearly towards electronic documentation.
EHR-integrated templates offer several advantages, including:
While less common, paper-based templates can be useful in situations where EHR access is limited. However, they are more prone to loss, damage, and illegibility.
Numerous examples of operative note templates are available online and through professional organizations. Searching for templates specific to your surgical specialty is recommended. Many hospitals and healthcare systems also provide their own standardized templates.
The operative note template is an indispensable tool for surgeons and healthcare professionals. By utilizing a well-designed template, you can ensure accurate, complete, and consistent documentation of surgical procedures. This not only improves patient care but also streamlines billing, reduces legal risk, and enhances communication within the healthcare team. Investing in a robust template is a crucial step towards optimizing surgical documentation and delivering the highest quality of care. Remember to regularly review and update your template to reflect changes in surgical techniques and best practices.