The healthcare landscape is constantly evolving, demanding efficient and organized documentation for pediatric care. This is where the Pediatric Soap Note Template comes into play – a crucial tool for clinicians to effectively communicate patient information, track progress, and streamline workflows. A well-structured soap note provides a concise and readily accessible record of a patient’s visit, facilitating collaboration among healthcare providers and ensuring continuity of care. This article will delve into the purpose, benefits, creation, and best practices for utilizing a Pediatric Soap Note Template. Understanding its importance is paramount for ensuring optimal patient outcomes and operational efficiency within pediatric settings. Pediatric Soap Note Template is more than just a document; it’s a vital component of quality patient care.
The need for standardized pediatric documentation has grown significantly in recent years, driven by factors such as increased complexity of care, the rise of electronic health records (EHRs), and the increasing demand for patient-centered care. Traditional paper-based documentation often leads to errors, delays, and inefficiencies. A standardized format, like the Pediatric Soap Note Template, offers a significant improvement in these areas. It promotes clarity, consistency, and accessibility, ultimately benefiting both patients and healthcare professionals. The benefits extend beyond simple record-keeping; it fosters better communication, improves patient safety, and supports data-driven decision-making. Let’s explore how this template can be utilized effectively.
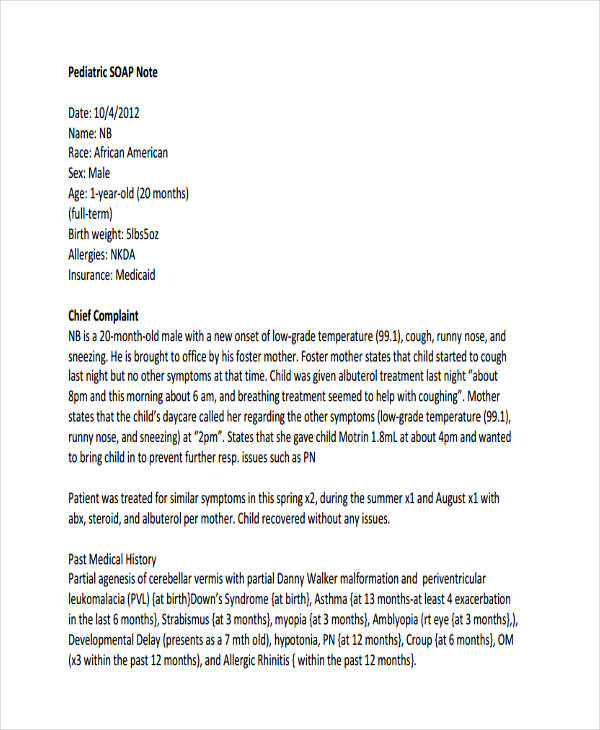
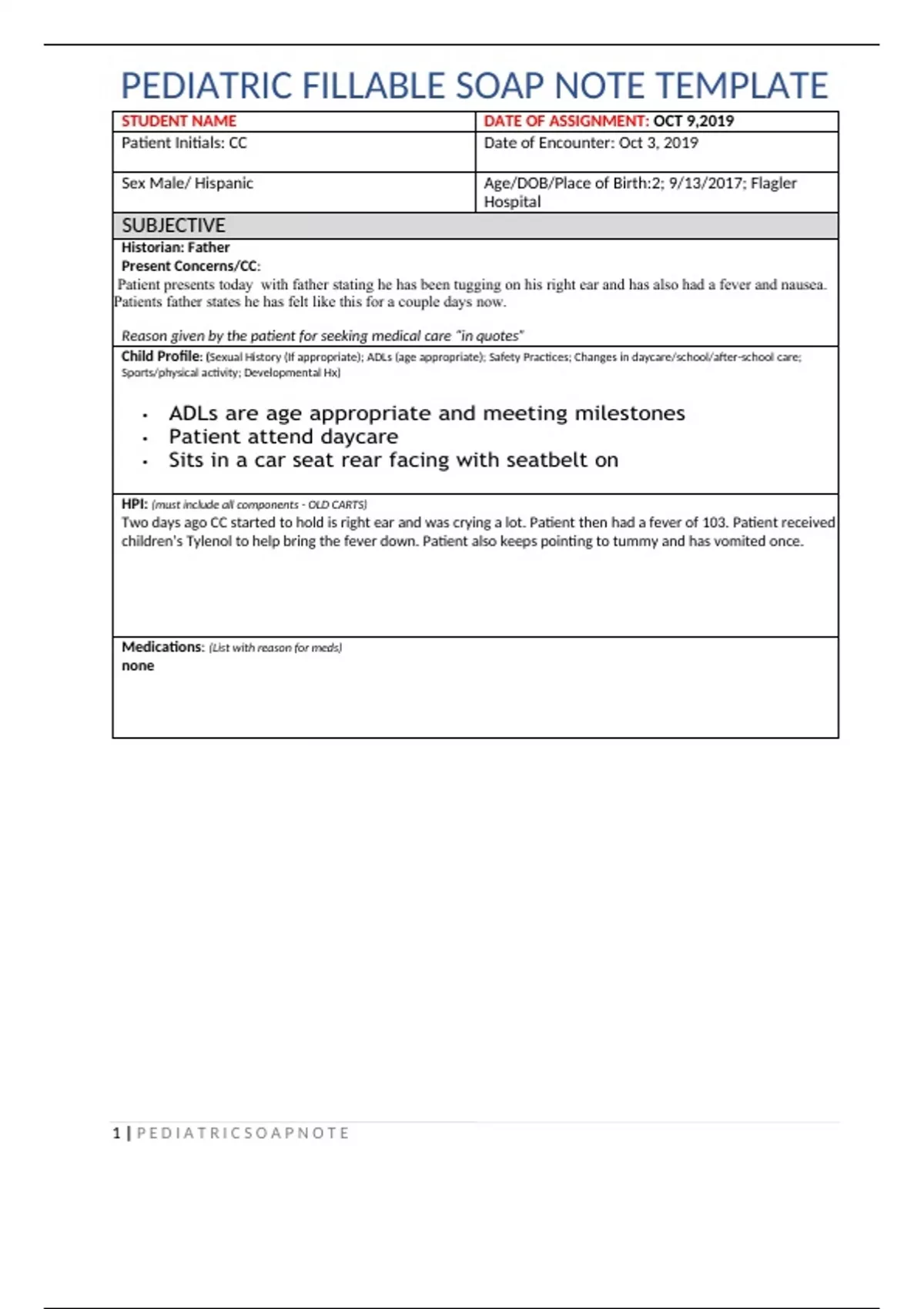
At its core, a Pediatric Soap Note Template is designed to capture essential information about a patient’s visit, particularly those related to pediatric care. It’s not simply a summary of the encounter; it’s a structured record intended to facilitate communication and collaboration. The template typically includes sections addressing vital details such as:
The specific sections and their order may vary slightly depending on the healthcare setting and the individual provider’s preferences, but the fundamental purpose remains consistent. A well-defined template ensures that all relevant information is captured consistently, reducing the risk of miscommunication and errors.
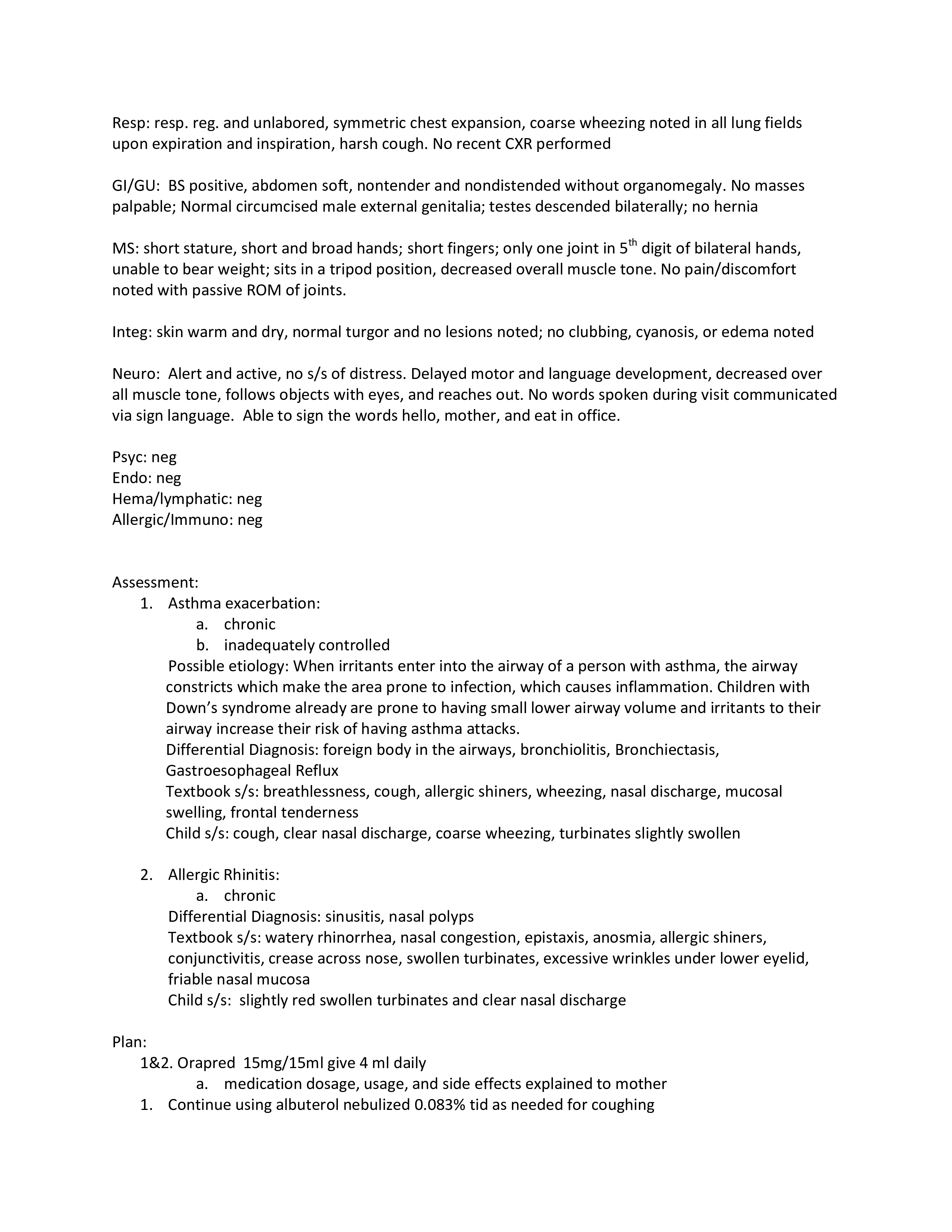
Let’s examine a typical section of a Pediatric Soap Note, illustrating how information is organized and presented. The “History of Present Illness” section is frequently the most detailed, requiring a thorough and chronological account of the patient’s symptoms and concerns. For example, a note might include: “Patient presents with fever (102°F) for 3 days, accompanied by cough and sore throat. Reports difficulty sleeping due to discomfort. Patient denies recent travel or exposure to illness.” This level of detail is crucial for identifying potential underlying causes and guiding appropriate diagnostic and treatment decisions. The “Assessment” section then summarizes the clinician’s observations and findings, often incorporating a brief physical examination summary. The “Plan” section outlines the next steps, ensuring a clear and coordinated approach to patient care.
Implementing a standardized pediatric soap note template offers a multitude of benefits for both patients and healthcare providers. Firstly, it significantly improves communication among team members, reducing the potential for misunderstandings and errors. Clinicians can quickly access a complete and accurate record of the patient’s history, leading to more informed decisions. Secondly, the template streamlines workflows, reducing the time spent on documentation and allowing providers to focus on patient care. This is particularly important in busy pediatric settings where resources are often limited. Thirdly, a well-structured template enhances patient safety by ensuring that all relevant information is captured consistently. Finally, it facilitates data collection and analysis, providing valuable insights into patient outcomes and identifying areas for improvement within the healthcare system. The use of a standardized format also contributes to improved billing accuracy and compliance with regulatory requirements.
Creating an effective Pediatric Soap Note Template requires careful planning and attention to detail. Several best practices can be employed to ensure its usability and effectiveness:
Technology is playing an increasingly important role in the creation and management of Pediatric Soap Notes. Mobile apps and electronic health record (EHR) systems are streamlining the process, allowing providers to capture and document patient information quickly and easily. These tools often include features such as automated note-taking, image capture, and integration with other clinical systems. Furthermore, automated templates and pre-populated fields can significantly reduce the time required to complete the note. The trend is towards a more integrated approach, where the soap note is seamlessly integrated into the patient’s electronic record.
The Pediatric Soap Note Template is an indispensable tool for pediatric healthcare providers. Its ability to streamline documentation, improve communication, and enhance patient safety makes it a critical component of quality patient care. By understanding the purpose, benefits, and best practices for utilizing this template, healthcare organizations can significantly improve the efficiency and effectiveness of their pediatric services. As technology continues to evolve, the role of the Pediatric Soap Note Template will only become more important. Ultimately, a well-utilized template contributes to a more organized, efficient, and patient-centered healthcare system. The continued adoption and refinement of this standard documentation practice will undoubtedly contribute to improved outcomes for children and families. Pediatric Soap Note Template remains a cornerstone of pediatric care, and its continued importance will only grow in the years to come.