The process of effective psychiatric care hinges on clear and concise communication between the patient and the clinician. A crucial element in this process is the utilization of a standardized template for psychiatric notes. A well-structured psychiatry note template provides a framework for documenting patient encounters, ensuring consistency, and facilitating seamless information sharing among healthcare providers. This article will explore the importance of psychiatry note templates, their various components, and best practices for their effective use. Psychiatry Note Template is more than just a document; it’s a vital tool for patient care and professional accountability. It’s a cornerstone of collaborative treatment planning and data collection, ultimately contributing to improved patient outcomes. Understanding how to create and utilize a robust template can significantly enhance the quality of care delivered.
The benefits of utilizing a standardized psychiatry note template are numerous and far-reaching. Firstly, it promotes consistency in documentation, reducing the risk of miscommunication and ensuring that all relevant information is captured accurately. This consistency is particularly important when multiple healthcare professionals are involved in a patient’s care. Secondly, it streamlines the workflow for clinicians, allowing them to quickly access essential information during consultations and treatment planning. A pre-defined template reduces the time spent on note-taking, freeing up valuable time for direct patient interaction. Furthermore, a standardized template facilitates data analysis and tracking of patient progress, enabling clinicians to identify trends and adjust treatment plans accordingly. Finally, it enhances patient safety by providing a clear record of the encounter, reducing the potential for errors and ensuring that important information is readily available.
Several types of psychiatry note templates exist, each tailored to specific clinical needs and practice settings. Some are highly structured, requiring detailed information about the patient’s history, current symptoms, and treatment plan. Others are more flexible, allowing for a broader range of information to be included. The choice of template depends on the clinician’s preferences, the complexity of the patient’s case, and the specific goals of the care. It’s important to note that a template is a guide, not a rigid set of rules. Clinicians should adapt the template to fit their individual needs and the specific requirements of their practice. A good template should be easily adaptable and easily updated as needed.
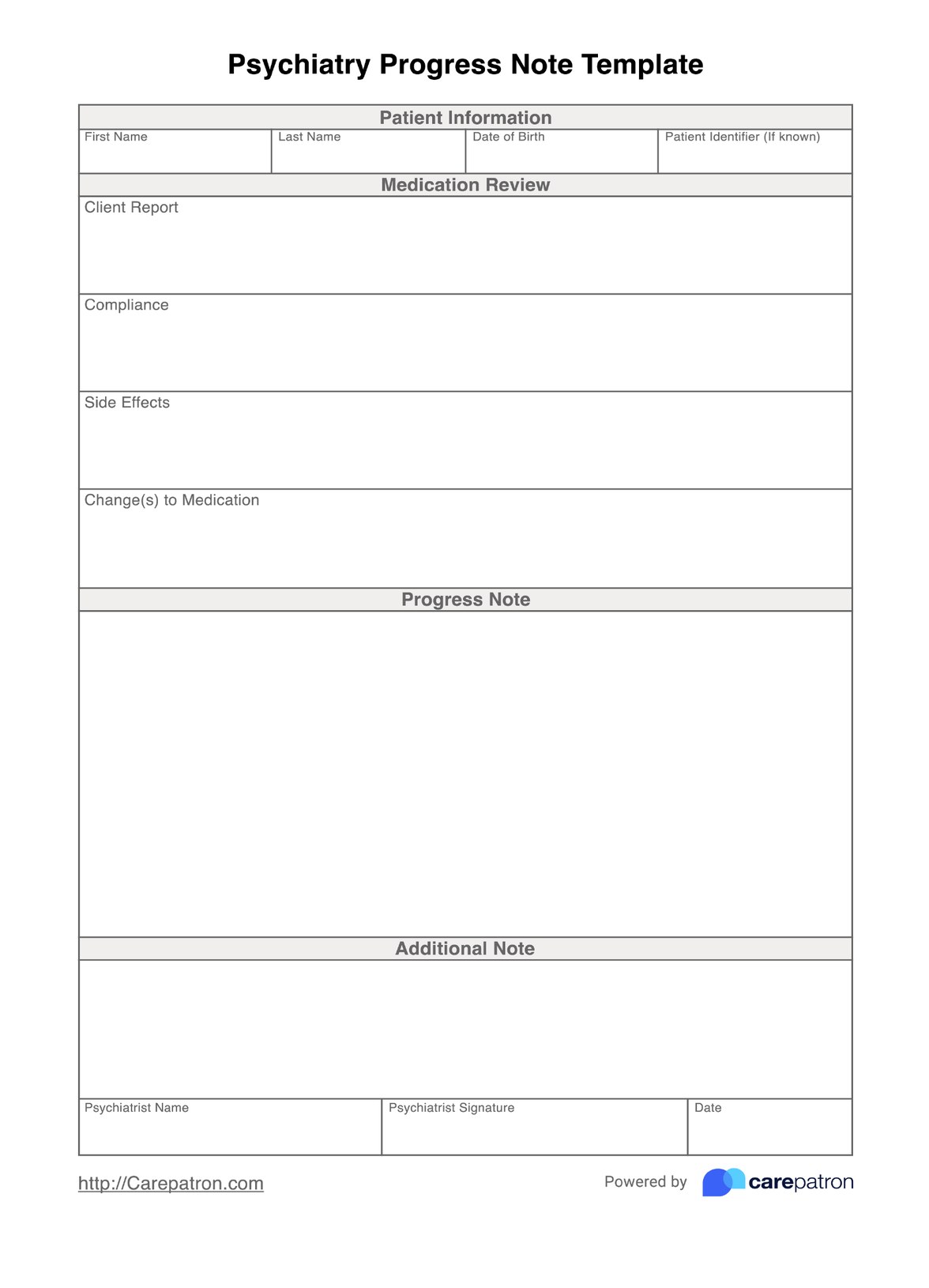
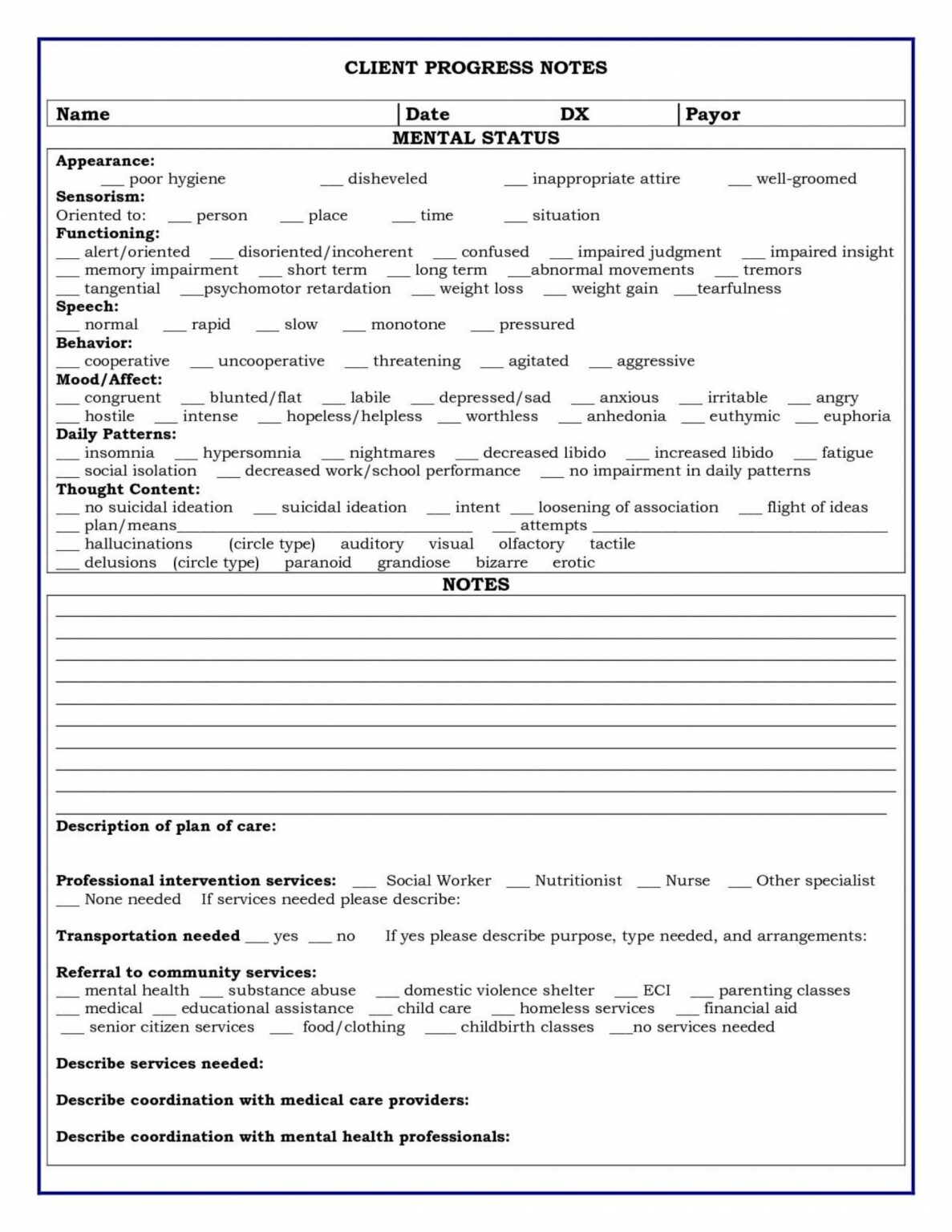
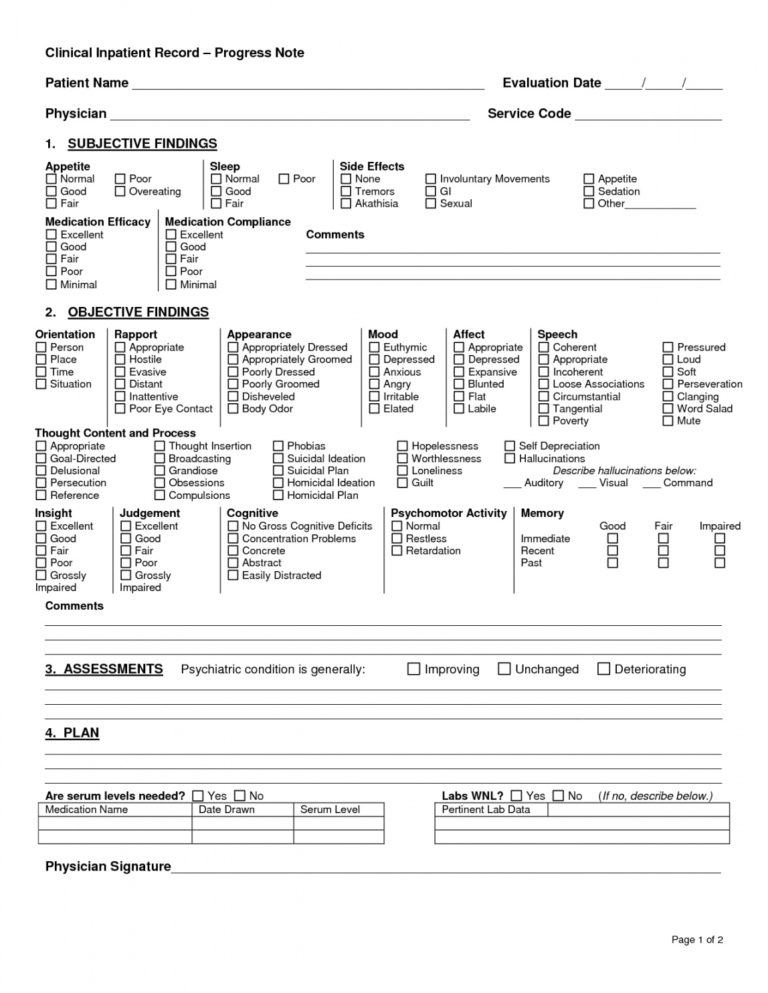
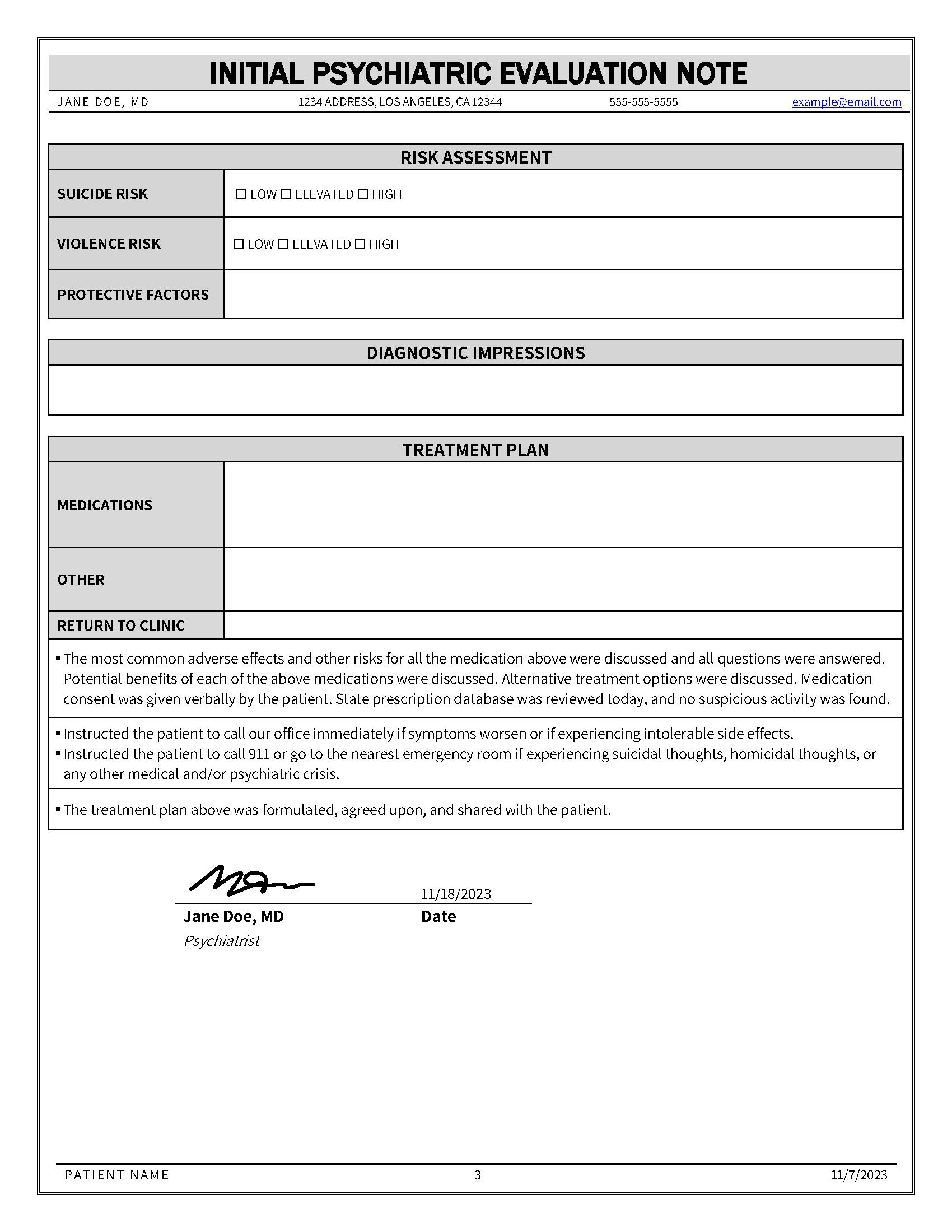
Let’s delve into the key components of a comprehensive psychiatry note template. A typical template will include sections for demographic information, chief complaint, history of present illness (HPI), psychosocial history, mental status examination findings, medication review, plan of care, and follow-up instructions. Each section will have specific prompts and fields to ensure that all relevant information is captured. The level of detail required in each section will vary depending on the complexity of the patient’s case. For example, a patient with a severe psychiatric disorder may require a more extensive HPI than a patient with a relatively mild anxiety.

This section gathers essential details about the patient, including:
This section captures the patient’s primary reason for seeking care. It’s a concise statement of the patient’s main concern.
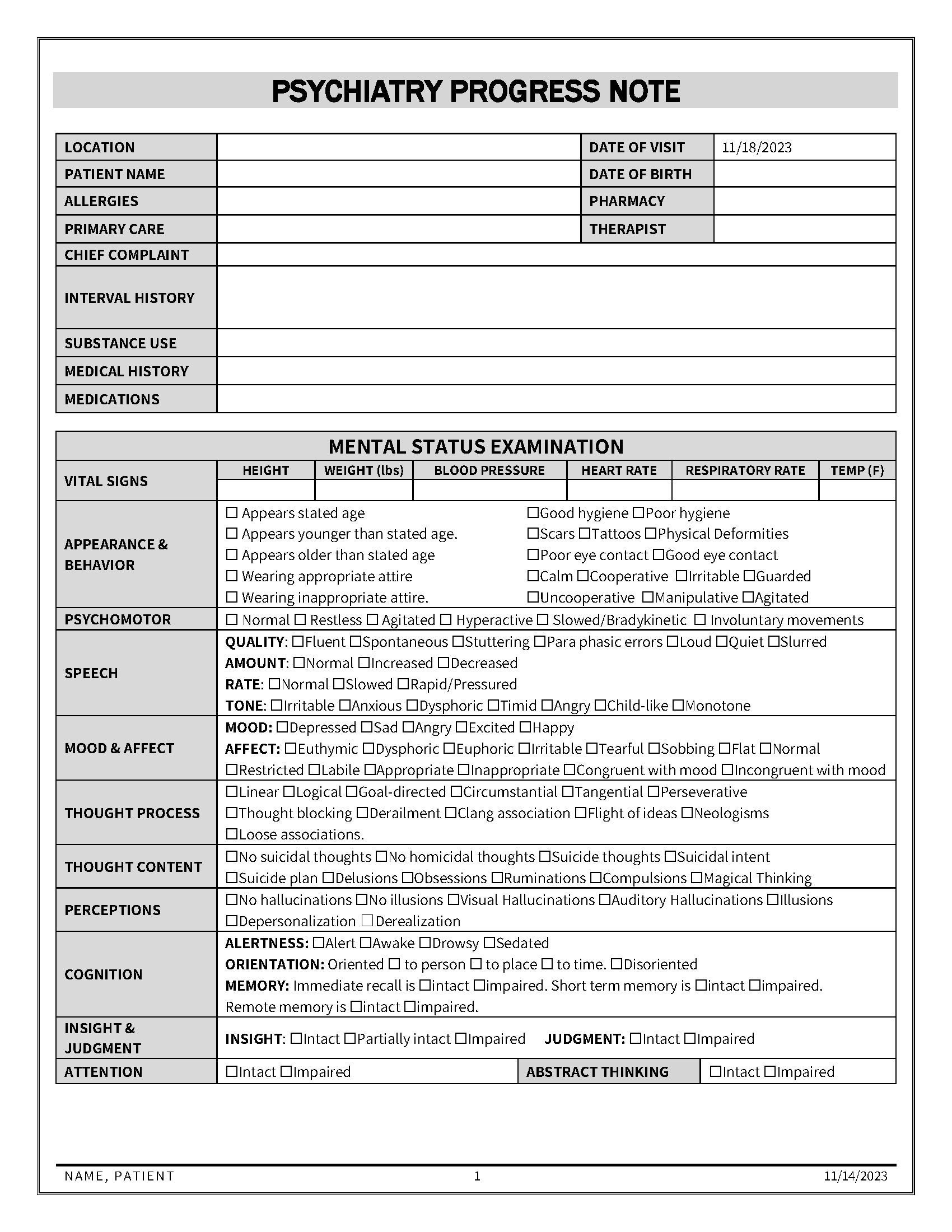
This section provides a detailed account of the patient’s current symptoms and concerns. It’s crucial for understanding the nature and severity of the patient’s condition.

This section explores the patient’s background, including their family history, social support, and significant life events. Understanding these factors can provide valuable insights into the patient’s current functioning.
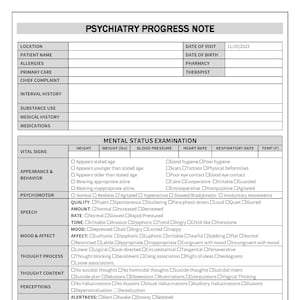
This section summarizes the patient’s mental status assessment, including observations about their awareness, orientation, mood, affect, thought process, and cognitive function.
This section documents the patient’s current medications, including dosage, frequency, and reason for taking them.

This section outlines the proposed treatment plan, including goals, interventions, and expected outcomes.
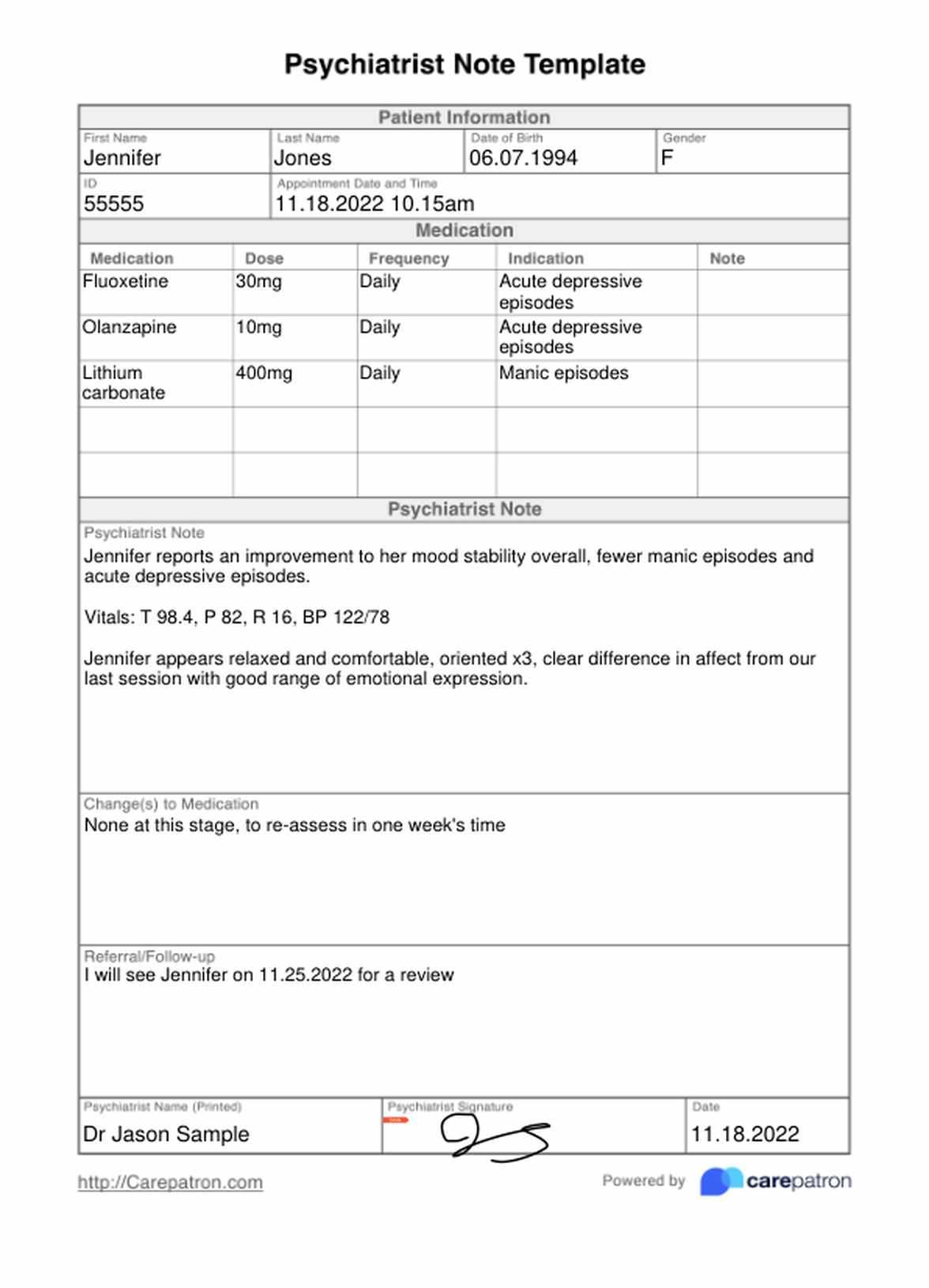
This section provides instructions for the patient and clinician regarding follow-up appointments and care.
This comprehensive approach to psychiatry note templates ensures that all relevant information is captured, facilitating effective communication and coordinated care. Regular review and updates of the template are essential to maintain its relevance and effectiveness.
The utilization of a well-structured psychiatry note template is a cornerstone of quality patient care. By providing a standardized framework for documentation, these templates streamline workflows, enhance consistency, and improve data collection. The benefits extend beyond simply documenting encounters; they contribute to improved patient safety, facilitate informed decision-making, and ultimately enhance the effectiveness of treatment. As healthcare practices evolve, the importance of a robust and adaptable template will continue to grow. Investing in the development and implementation of effective templates is a critical step towards delivering optimal patient care. The consistent application of a standardized template will undoubtedly contribute to a more efficient and patient-centered healthcare system.