The process of documenting a patient’s progress in a psychology treatment setting is a critical component of effective care. A well-structured psychology progress note provides a comprehensive record of the patient’s condition, interventions, and responses, facilitating continuity of care and informed decision-making. This article will delve into the essential elements of a robust psychology progress note template, offering guidance on its creation and effective utilization. Psychology Progress Note Template is more than just a document; it’s a vital tool for maintaining patient safety and optimizing treatment outcomes. Understanding its nuances is paramount for any clinician involved in psychological care.
A psychology progress note isn’t simply a summary of what happened during a session. It’s a detailed account of the patient’s experience, their emotional state, and how the treatment has impacted them. It’s a crucial tool for tracking progress, identifying potential challenges, and adjusting treatment plans accordingly. Without a clear and comprehensive record, it’s difficult to assess the effectiveness of interventions and ensure that the patient is receiving the appropriate care. Furthermore, it’s essential for legal and ethical reasons, providing a documented history for patient records and potential legal proceedings. The ability to accurately and thoroughly document a patient’s journey is a cornerstone of ethical and effective practice.
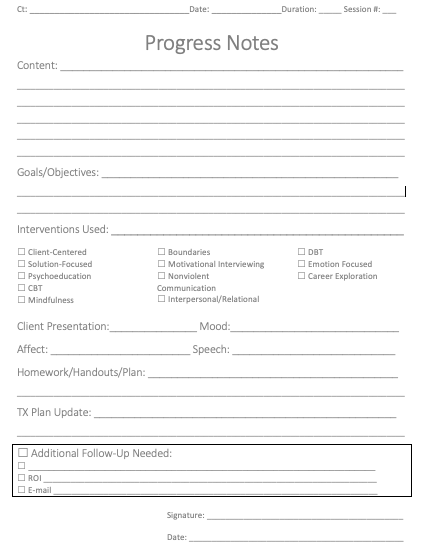
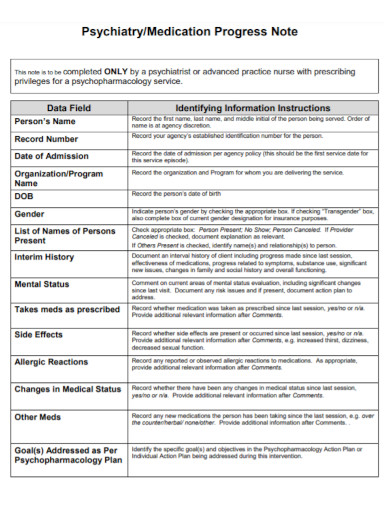
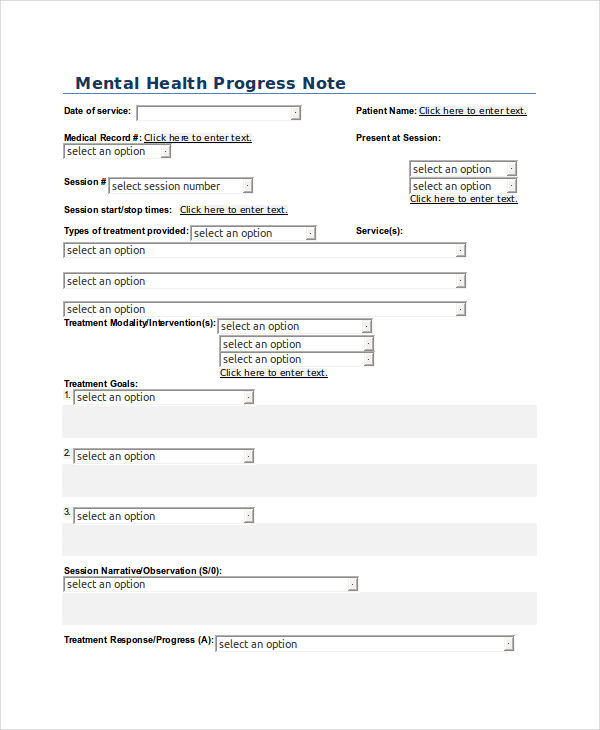
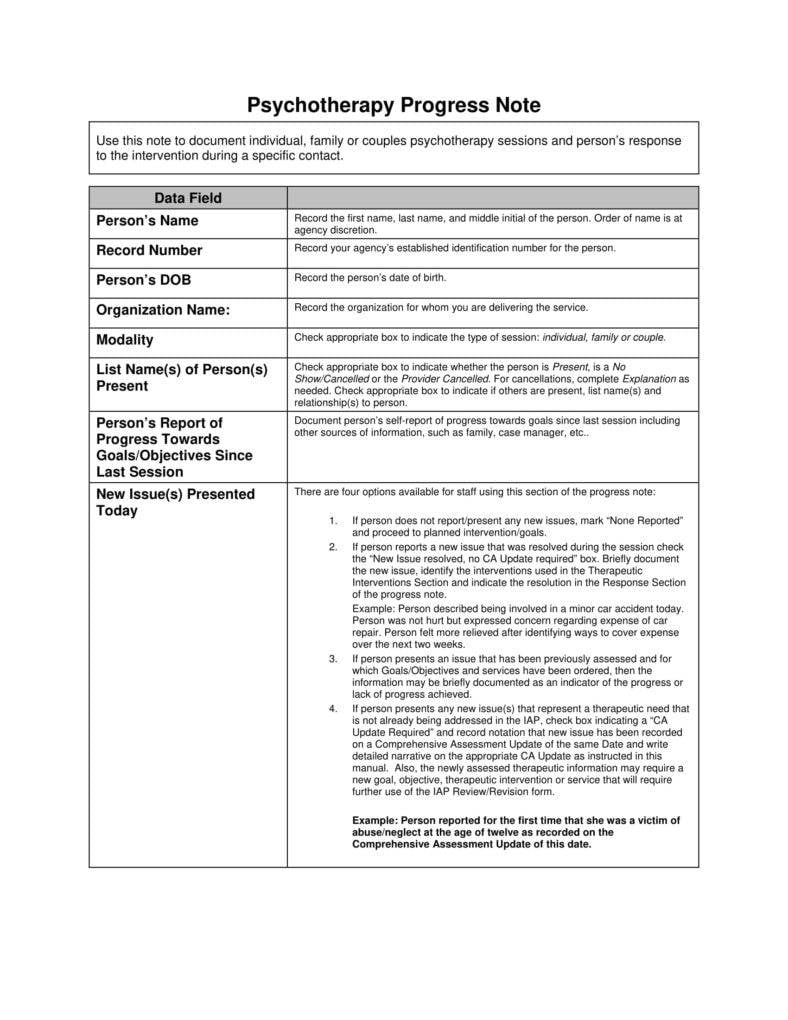
A complete psychology progress note typically includes several key sections. Each section serves a distinct purpose and contributes to a holistic understanding of the patient’s condition. The following are some of the most important components:
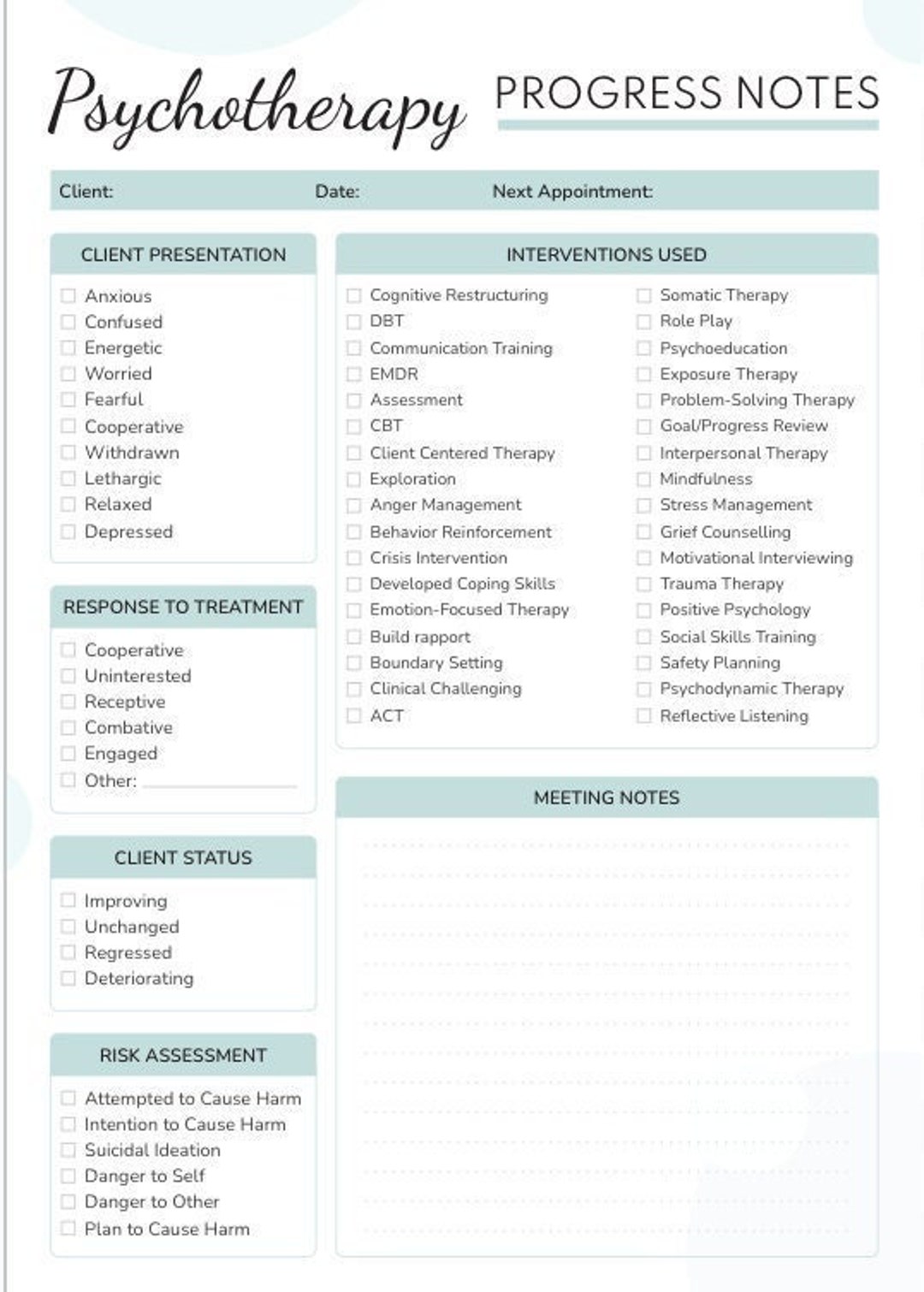
Creating a truly effective psychology progress note requires careful attention to detail and a systematic approach. Here are some tips for maximizing its utility:
While paper progress notes remain a standard, electronic progress notes are increasingly prevalent. Electronic systems offer several advantages, including improved data security, enhanced accessibility, and the ability to track patient information more efficiently. However, it’s crucial to ensure that electronic systems are properly integrated with existing clinical workflows. The key is to leverage technology to support the progress note process, not replace it entirely.
Progress note documentation can be challenging, particularly when dealing with complex or sensitive cases. Some common challenges include:
Addressing these challenges requires providing clinicians with adequate training, support, and resources. Implementing robust data security protocols and adhering to ethical guidelines are also essential.
The future of progress note templates is likely to involve greater integration with electronic health records (EHRs) and the use of data analytics to identify trends and patterns. AI-powered tools may also play a role in automating some aspects of progress note documentation, freeing up clinicians to focus on patient care. The goal is to create progress notes that are not only accurate and comprehensive but also readily accessible and easily searchable, ultimately enhancing the quality of care.
A well-structured psychology progress note is an indispensable tool for effective patient care. By understanding the core components, utilizing best practices, and addressing potential challenges, clinicians can create progress notes that provide a comprehensive and reliable record of a patient’s progress. The continued evolution of technology and the increasing emphasis on data-driven decision-making will undoubtedly shape the future of this vital documentation practice. Psychology Progress Note Template remains a cornerstone of clinical practice, requiring careful attention and consistent application to ensure optimal patient outcomes.

The process of documenting a patient’s progress in a psychology treatment setting is a critical component of effective care. A well-structured psychology progress note provides a comprehensive record of the patient’s condition, interventions, and responses, facilitating continuity of care and informed decision-making. A complete and detailed progress note is essential for tracking progress, identifying potential challenges, and adjusting treatment plans accordingly. The ability to accurately and thoroughly document a patient’s journey is a vital tool for ethical and effective practice. Ultimately, the quality of the progress note directly impacts the patient’s well-being and the clinician’s ability to provide optimal care. The consistent use of a standardized template, coupled with ongoing training and a commitment to data security, is key to maximizing the value of this critical documentation tool.